This is a shallow report examining loneliness.
In a nutshell
|
Key uncertainties
The current interventional evidence base is predominantly cross-sectional or short in duration, marked by relatively small and not globally representative samples, so it is hard to make strong causal claims as well as claims with high certainty for generalizability. There are few longitudinal interventions, so little is known about the long-term impacts and potential sustainability of such projects.
Some of the promising interventions to tackle loneliness require significant involvement in terms of time and service provision, and so may be difficult to scale. Compounding this difficulty, many of the most socially isolated people live rurally or in poorly connected areas and so reaching them may be challenging.
A surprising key target many current anti-loneliness interventions miss is actually recruiting participants who are lonely. I anticipate this is an essential part to understanding the real cost-effectiveness of available interventions. Beyond this, provision of a relevant intervention type for the relevant group as well as provision for a sufficient length of time are also warranted. |
Importance
Problem Overview
Question | Answer |
Definition of the problem | Loneliness is commonly defined as a discrepancy between a person’s desired and actual social relationships or opportunities for social contact. This can be a subjective (perceived) or objective discrepancy (social isolation). Loneliness is a risk factor for a variety of general and mental health conditions, mortality, loss of productivity, and poor self-esteem. |
Burden of the problem | Health burden:
Productivity burden:
Wellbeing burden:
I note the difficulty in providing global burden estimates as almost all data comes from high income settings and we know little about the distribution of loneliness and its impacts in LMICs, where healthcare costs also tend to be markedly different. |
Who is affected at what point in their life | Gender of people affected: Both men and women. Age of people affected: Tends to be more common in older age (though possible at any age). Situation in which they are affected: Experiencing social isolation, living alone, having fewer opportunities for social contact, becoming widowed, having poor health and chronic health problems, especially in older age. |
Introduction to the problem
Loneliness is commonly defined as a discrepancy between a person’s desired and actual social relationships or opportunities for social contact (Russell, Peplau, & Cutrona, 1980). This can be a subjective discrepancy (perceived loneliness) or objective discrepancy (social isolation). Loneliness should be distinguished from merely being on your own and related concepts such as solitude, defined as a state of internal focus (Weinstein, Hansen, Nguyen, 2022).
Loneliness is a risk factor for a variety of general and mental health conditions, mortality, loss of productivity, and poor self-esteem among others. The mechanisms and quality of evidence tying loneliness and different conditions are varied ranging from very strong and likely causal (e.g. impacts on depression) to still poorly understood and mostly correlational (e.g malnutrition, inflammation).[2]
There is some discussion about whether or not loneliness has been increasing. One recent meta-analysis (k=345) suggests this might be the case; for emerging adults (n=124,855) over the last 43 years, loneliness has been increasingly with each calendar year (b=0.224, 95%CI [0.138, 0.309]), corresponding to 0.56 standard deviations on the UCLA loneliness scale (Buecker et al., 2021).[3]
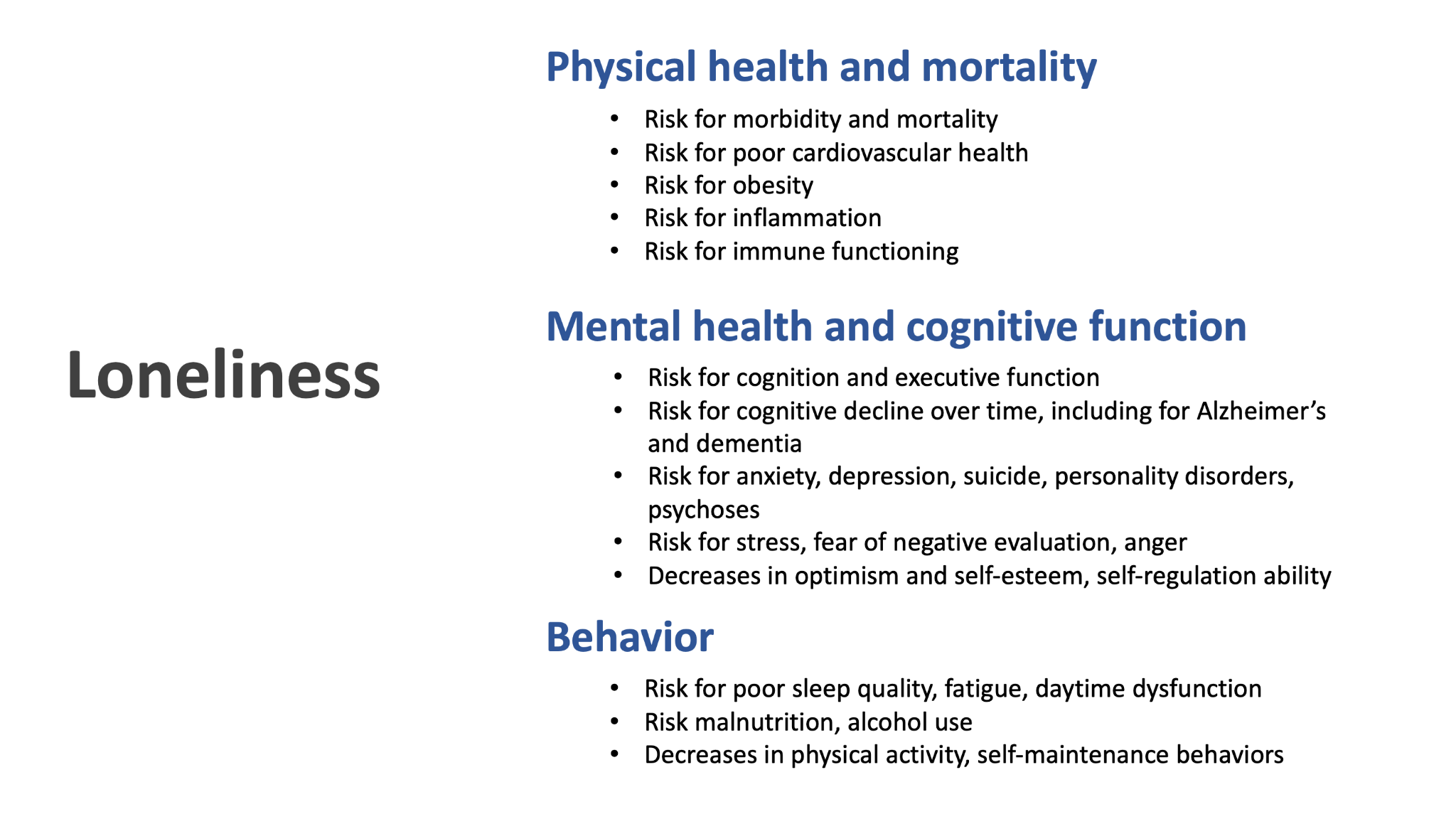
Quick outline of loneliness as a multi-domain risk factor based on a literature review.
What parts or aspects of loneliness carry the greatest risk or are most associated with the heaviest burden?
Severity
One meta-analysis (k=70) examined the impacts of social isolation (defined as a pervasive lack of social contact or communication, participation in social activities), loneliness (defined as experiencing feels of isolation, disconnectedness, and not belonging) and living alone (measured as a binary yes/no item) on mortality. After adjusting for potential confounds, the weighted average effects size were: social isolation odds ratio (OR = 1.29, loneliness OR = 1.26, and living alone OR = 1.32), corresponding to an average of 29%, 26%, and 32% increased likelihood of mortality (Holt-Lunstad et al., 2015). While these numbers are fairly similar, they would still coarsely suggest that greater levels of isolation carry a greater burden for mortality. Another review focusing on the economic toll of loneliness (k=12) similarly found that social isolation was associated with higher economic costs than loneliness (Mihalopoulos et al., 2019). Social isolation seems well established as a risk factor for all cause mortality based on a recent meta-analysis with data from 1.3 million individuals (hazard ratio 1.33 (95% confidence interval; 1.26-1.41, heterogeneity: Chi² = 112.51, P < 0.00001, I² = 76% ) Naito et al., 2023).
Frequency
One longitudinal 50-year study (n=7,638) suggested both situational and chronic loneliness were associated with higher risks for all cause mortality, with chronically lonely individuals (HR = 1.83; 95% CI: 1.71–1.87) exposed at slightly greater risk for mortality than those who were only situationally lonely (HR = 1.56; 95% CI: 1.52–1.62; Shiovitz-Ezra & Ayalon, 2009).
In another study, involving a 4 year follow-up (n=2,390), for both transiently lonely and chronically lonely people there were negative significant general health impacts (e.g. vision, mobility, self-care; Martín-María et al., 2019). Here, too, chronically lonely people had worse health than transiently lonely individuals (transient: β = −0.063 and chronic: β = −0.075, p < 0.001). Another study (n=2,995, 6 year follow-up) supports this pattern, where both transiently and chronically lonely people reported worse cognitive function, with the chronic loneliness being associated to more pronounced negative cognitive impacts (transient: β = −0.389, t = −2.191, df = 2994, p = 0.029; chronic: β = −0.640, t = −2.109, df = 2994, p = 0.035).
In summary, the evidence suggests that experiencing loneliness, regardless of severity or frequency, likely will bear negative implications for health, although the greatest burden of health problems will be experienced by those reporting chronic loneliness and the most severe levels of loneliness or isolation.
Sociodemographic and geographic distribution of the problem
Prevalence of loneliness across the globe
It is still not robustly clear how common and widespread loneliness is worldwide. Suboptimal measurement practices and lack of data prevent the robust estimation of the prevalence of loneliness.
Estimates from individual surveys vary, notably some are as high as 40-45%. For instance, reports by the UK’s Campaign to End Loneliness suggest about 45% of adults experience loneliness occasionally, sometimes or often, which would translate to about 25 million people in England (where the survey was done). Although this estimate is likely a high-end estimate, if we scale this globally, this would mean approximately 1.26 billion adults experience loneliness at least sometimes (taking 45% of UN statistics that 2.8billion people are now aged 40 or above). At a more conservative level of 20%, this would mean 560 million adults globally.
When we focus only on the most problematic forms of loneliness (severe or very frequent), there is high quality available evidence from a recent series of meta-analyses in 113 countries. There is a good degree of variance in the prevalence of evere of frequent[4] loneliness amongst age groups and countries, ranging from about 9% for adolescents, to 3%-7% for adults in Northern European countries and 8%-24% for adults in Eastern European countries. Data for adolescents were available globally, but for all other age groups (i.e. children and adults) data was not available anywhere outside of Europe.
Limited longitudinal data suggests there may be cultural variances in how loneliness is understood in older age. In surveys of adults aged 65+, prevalence rates of loneliness between 25.3% - 32.4% were found in Latin America (Cuba, Dominican Republic, Venezuela, Peru, Mexico), 18.3% in India, and a much lower rate of 3.8% in China (Gao et al., 2021). Notably, there was a robust association between loneliness and mortality in Latin America and China, but there was no such association in India, suggesting the further need for global surveys of loneliness and health.
A key recommendation for funders and academics is to incorporate validated loneliness measures across ages into general health surveillance efforts. We are currently limited in what we can say about the prevalence and distribution of loneliness in LMICs.
Who faces the highest risk of being lonely?
Who should loneliness interventions and services target? In sum, this section suggests that focus is warranted on those who have recently been widowed or have poor health. Interventions should target both men and women, most likely targeting older populations, although evidence is mixed with some suggesting young people may also be facing higher risks.
Older age seems to track with increases in loneliness (with caveats)
- Loneliness seems to be experienced more often in later age, particularly after 65 (Nicolaisen & Thorsen, 2014; Dykstra, van Tilburg, & de Jong Gierveld, 2005 & 2016). However, there is nuance in understanding the importance of age and the evidence base is overall mixed in terms of quality and findings.
- In a meta-analysis examining the impacts of loneliness on mortality, lonely middle-aged adults (<65) were at highest risk for mortality (looking only at the impact of loneliness on mortality from disease; this meta-analysis excludes death by accident or suicide; Holt-Lunstad et al., 2015) rather than the older adults. One possible explanation may be that individuals who live longer are more resilient, with different social or health characteristics. Alternatively, it may be that sociocultural factors are relevant, such that the decrease in one’s social network is seen as more normative with increased age, which may lead to different risks being associated with loneliness. One study found that lonely retired people were at risk for anxiety and depression but not physical health (chronic conditions; Bekhet and Zauszniewski, 2010). In either case, it seems that relevant confounders may underpin the relationship between age and loneliness.
- Importantly, there is a small body of work that suggests that the relationship between loneliness and age could be U-shaped, such that younger and older people face the highest risk (Victor & Yang, 2012). Nicolaisen & Thorsen, 2014 also found differences underpinned by measurement choices, such as when direct measures of loneliness were used, both the oldest (65-81) and the youngest (18-29) reported experiencing loneliness most often, but when indirect measures were used there was an overall positive association between age and loneliness, such that the older people were, the more lonely they tended to be.
- Some scholars have previously suggested individual-level traits or behaviors may be relevant as well. For instance, de Jong Gierveld (1998) suggests that personality characteristics are more important in younger people than older people for loneliness. New work is emerging in the context of social media and technology changes as well.
The effect of gender on loneliness is inconclusive
- Current research tentatively suggests that differences in loneliness reporting between men and women may be underpinned by measurement selection (Nicolaisen & Thorsen, 2014). In particular, direct or indirect measures of loneliness seem to lead to differences in reporting, such that overall (combining measures) the prevalence rates are similar for men and women, but when direct measures are used, loneliness is more prevalent for women, and when indirect measures are used, loneliness is more prevalent for men. There is a limited evidence base examining measurement carefully, so this finding should be interpreted cautiously.
- There may be some gender differences when trying to measure loneliness or social isolation. For instance, 14% of older men experienced moderate to high social isolation compared to 11% of older women (Beach & Bamford, from ILC-UK). Caution should still be applied, as differences tend to be small and some have argued measures of social isolation, that track contact with friends or family, can serve as a form of indirect measure for loneliness. A further meta-analysis (n= 398, 338; k = 634 studies; 747 effects size) attempting to tease apart potential gender differences in loneliness showed a close to zero-overall effect of gender, suggesting that mean levels of loneliness are similar for men and women across the lifespan (Maes et al., 2019)
- A nationally representative study in the UK indicated that gender was not independently associated with loneliness when confounding influences of marital status, age, and living arrangement were excluded (Victor et al., 2005). In an unadjusted model, women were more likely to be lonely. Women were significantly more likely to be widowed, live alone, but also more likely to have direct contact with friends and relatives. This aligns with research from older people in Sweden that suggests that while older men and women may share some risk factors for experiencing loneliness, they also have unique risk factors (Dahlberg et al., 2014).
- Overall, at present, it seems the main effect of gender and the interaction of age and gender do not differentiate higher risk groups for loneliness. Rather, a more careful consideration of other present confounders is pertinent. It is then important to recognize the different sociocultural experiences of people from different genders that may serve as particular risk factors (i.e. older women who are widowed, as well as those living alone; older men who have little social contact).
Becoming widowed is one of the strongest risk factors
- A varied body of literature (de Jong Gierveld & van Tilburg 1987; Pinquart 2003; Stroebe & Stroebe 1987; Victor et al. 2005) indicates that losing your partner is an important risk factor for becoming lonely. This is especially so for older adults. Older adults who become widowed showed the greatest increase in loneliness in one 7-year longitudinal study from the Netherlands (Dykstra et al., 2016) and in other analyses (Nicolaisen & Thorsen, 2014). Women are more likely to experience widowhood.
Poor health: a risk factor and part of a vicious cycle
- Being in poor health, across a variety of measures, seems robustly associated with experiencing loneliness (Nicolaisen & Thorsen, 2014). Crucially, loneliness seems to be a risk factor for poor health across different domains as well, thus potentially leading to the formation of a vicious cycle.
How big is the problem?
Key reviews about the economic costs of loneliness: Mihalopoulos et al., 2019 and McDaid, Bauer, & Park (2019). Both reviews point to a limited evidence base, a difficulty to compare results because of the heterogeneity of methods, and challenges associated with measurement practices. The vast majority of evidence comes from the UK (more than 50% of the papers found in both reviews).
Economic burden of loneliness
UK: Burden on health
- Fulton & Jupp (2015) estimate the cost of being chronically lonely of £11,725 per person over a medium term of about 15 years (or about £780 per annum per person), compared to people who are not lonely. Their work suggests about 40% of the cost occurs within the first 5 years of being lonely and around 20% is linked to residential care. In this research, people who were lonely reported 1.3-1.8 times higher rates of accessing healthcare services and were also at increased likelihood for developing health conditions requiring further care.
- To compare this figure, the annual cost of coronary heart disease per person in the UK is £597, for breast cancer it is £651, and for hypertension it is £807 (Public Health England, 2020).[5]
- McDaid et al. (2021) estimate a £1700 net present value cost per person over 10 years (£170 per annum per person) or £6000 if only considering those reported being lonely most of the time. Being even slightly lonely at baseline was associated with more frequent use of GP services at follow-up. At each follow-up wave of the survey being lonely was linked to significantly higher rates of using community nursing and ‘meals on wheels’ services.
- McDaid et al. focus on 50+ in the UK, which equals approximately 25.75 million people (Statista based on ONS), of which 2 million are likely long-term lonely (Campaign to End Loneliness). This would mean an annual cost £340 million in the UK
- If we take the Fulton & Jupp annual cost estimate (£780), that would mean a total annual cost of £1.56 billion in the UK.
- For reference, and to make this number more comparable with some context, in 2021 the UK spent £11.4 billion on global aid. The cost of loneliness in the UK is just over 10% of the country’s global aid portfolio.
- A UK report by Peytrignet et al. (2020) supports the figure of £600 per year (2015 prices) or £672 (2019 prices) when looking at healthcare costs for those affected by loneliness most of the time.
- Notably this report offers higher numbers for the impact on wellbeing, such that the annual wellbeing impacts of loneliness are £6,429 for those reporting mild loneliness and at least £9,976 for those reporting moderate to severe loneliness. These estimates exclude health and productivity impacts.
UK: Productivity loss
- A report by the Co-op suggests a total annual loneliness cost to UK employers of £2.5 billion, which breaks down to
- £20 million in sickness absences
- £220 million in lost working days caring for someone who is ill due to loneliness
- £665 reduced productivity costs
- £1.62 billion in costs associated with increased voluntary staff turnover
USA
- In the States, Shaw et al. (examined older adults >65) and reported that socially isolated people incur higher annual healthcare costs of about $1643 more than people who have social networks of support. This was particularly salient for women who were both widowed and isolated compared to women who were not isolated with a cost increase of $3276.
- The US Census Bureau, there are about 56 million adults aged 65 and over in the USA. Conservatively assuming 20% are lonely, this would mean that there are 11.2 million lonely adults, and incurring additional healthcare costs of $18.4 billion linked to their loneliness.
Australia
- A report by Bankwest Curtin Economics Centre estimates a total annual cost of loneliness in Australia at $2.7 billion a year, equivalent to $1,565 for each person who becomes or remains lonely. A greater share of the overall costs of loneliness comes from impacts on women (59%). The total amount is broken down in:
- $863 million in greater incidence of smoking
- $833 million in higher number of GP visits
- $379 million associated with greater physical inactivity
- $344 million in excessive alcohol consumption
Loneliness & Life satisfaction: how many WELLBYs are lost due to loneliness?
Being lonely has significant negative impacts on life satisfaction. I use such estimates from research to approximate the cost of being lonely in terms of WELLBY lost. A WELLBY is equal to a one-point change in life satisfaction (when measured on a 0-10 scale) per person per year (see further e.g. De Neve et al, 2020).
- Peytrignet et al. (2020)’s report examines the impact of loneliness on life satisfaction and finds on the basis of two UK surveys and find that any level of loneliness is associated with decreases in life satisfaction.[6] In particular, I’m drawing numbers from their technical supplement.[7]
- Using the Community Life Survey, where being lonely is measured on a 5 point scale from ‘Never’ to ‘Often/Always,’ the impacts are as follows in the table below (where the first two columns are directly from the report). The estimates are controlled for year of interview, household size, household income, sex, age, marital status, economic status among others.
- For the purposes of this shallow report, I’m interested in an initial approximation of country-level WELLBYs lost and will not add time discounting but I note fluctuations year-to-year seems to be less than 5% and there is further guidance on how to incorporate annual changes and discounts from the Social Impacts Task Force.
- To estimate the population-level WELLBYs lost, I am using estimates from the ONS about how many people experienced different levels of loneliness in the same year as the report (2020), though as this year includes some of the lockdowns during the Covid-19 pandemic in the UK, they are likely not generalizable and possibly overestimates.[8]
Loneliness level (all compared vs Never lonely) | Coefficient (Marginal impact on life satisfaction) | Impact in terms of WELLBY lost (rounded) | UK population | Total WELLBYs lost in UK |
| Often/Always | -1.964 | 2 | 1.9 million adults | 3.8 million |
| Some of the time | -1.0398 | 1 | 4 million adults | 4 million |
| Occasionally | -0.688 | 0.7 | 9 million adults adults | 6.3 million |
| Hardly ever | -0.266 | 0.3 | 8.9 million adults | 2.67 million |
| Total | 16.77 million |
- The other estimates in this report come from the Understanding Society survey (measures only ‘Often’ or ‘Some of the time’ lonely), and are similarly controlled for a number of relevant variables (e.g. life satisfaction in previous survey waves, economic status, gender, age etc.)
Loneliness level (all compared vs Hardly ever / Never lonely) | Coefficient (Marginal impact on life satisfaction) | Impact in terms of WELLBY lost (rounded) | UK population | Total WELLBYs lost in UK |
| Some of the time | -0.418 | 0.4 | 4 million | 4.4 million |
| Often | -1.134 | 1.1 | 3.8 million | 4.18 million |
| Total | 8.58 million |
- Layard et al. (2020) estimate the loss of one year’s life as 7.5 WELLBYs lost. If we take the more conservative estimate of 8.58 million WELLBYs lost annually due to loneliness, this would equate to 1,144,000 (1.14 million) years lost annually in the UK.
- The average life expectancy in the UK is about 81 years, so this would mean 14, 123 lives lost annually attributable to loneliness.
How effective are interventions addressing loneliness and social isolation?
- Overall, there is some evidence for effectiveness based on a rich body of systematic reviews. I note a lot of variance and relatively small samples. It is hard to assess which intervention types are most effective.
- Many systematic reviews comment that the majority of included studies do not explicitly target people who are lonely. I note in many cases services are provided to a particular population where the mechanism of the intervention does not seem as the most theoretically appropriate route for change. Few interventions provide theoretical basis for their research designs or services (see further Bessaha et al., 2020)
- A meta-analysis of interventions aiming to reduce loneliness by Masi et al. (2011) supports the effectiveness of interventions aiming to alleviate loneliness. Interventions were categorized into four main intervention types, those that 1) improve social skills, 2) enhance social support, 3) increase opportunities for social contact, and 3) address maladaptive social cognition. A moderator analysis with intervention type was carried out in single group pre-post studies, where intervention type could not explain difference in effect size (i.e. did not provide evidence that, for instance, addressing maladaptive social cognition was more effective than improving social skills etc.) There was notably heterogeneity in interventions and participant populations.
- When looking at the included randomized group comparisons, Masi & colleagues noted effect sizes that were smaller than would be anticipated in social and behavioral interventions. A meta-analysis of 302 social and behavioral interventions (Lipsey & Wilson, 2001) showed that on average interventions generate a mean effect size of 0.50. Masi & colleagues estimate that their mean effect size of loneliness interventions, -0.198 would be around ‘the bottom 15% of the distribution” of effects in the broader field of social and behavioral work, pointing to a lower degree of efficacy. This likely speaks to the difficulty in providing effective loneliness interventions.
What are the most common interventions?
Befriending interventions
In these interventions, a ‘befriender’ visits or contacts a lonely person (e.g. in their home, a designated space, remotely). Befriending interventions are not typically structured and tend not to have formally defined goals either for each interaction or the overall course of the befriending sessions, but tend to prioritize the development of informal and natural contact. Befrienders may have received prior training (more often the case when providing care to patients with other conditions, e.g. dementia) or may be volunteers. Some interventions will try to match people by common interests or preferences.
According to one systematic review, compared to usual care (commonly no intervention) befriending has a small but significant effect on depressive symptoms in the short-term (standardized mean difference SMD=−0.27, 95% CI −0.48 to −0.06, nine studies) which likely decays over time, as evidenced by smaller effect sizes over the long term (SMD = −0.18, 95% CI −0.32 to −0.05, five studies; Mead et al, 2018). This review further pointed out that the current effective evidence for befriending interventions does not meet the National Institute for Health and Clinical Excellence’s depression guidelines for adoptions (SMD of 0.5 or more).
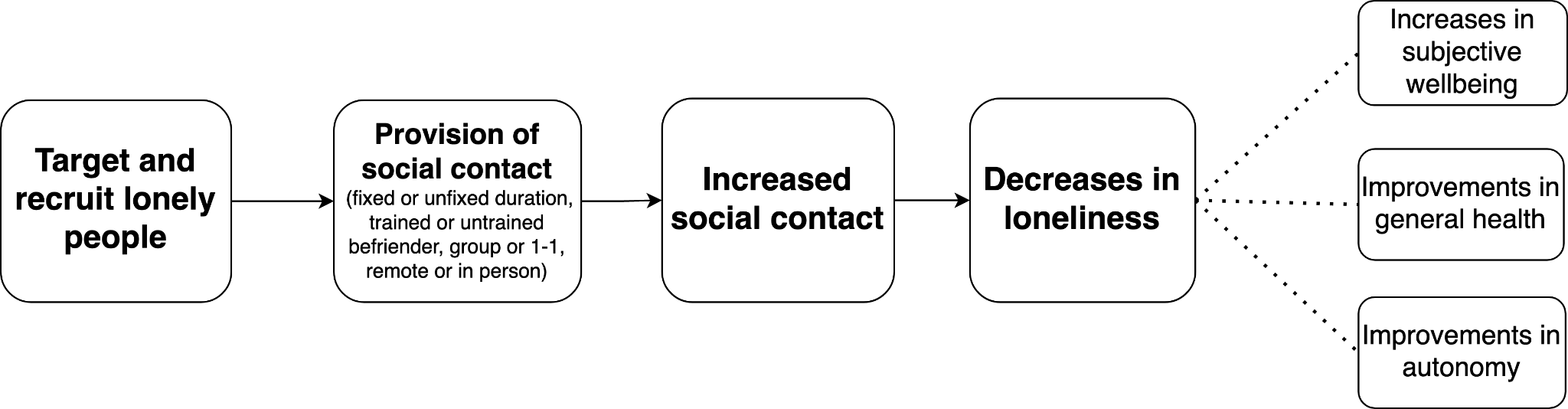
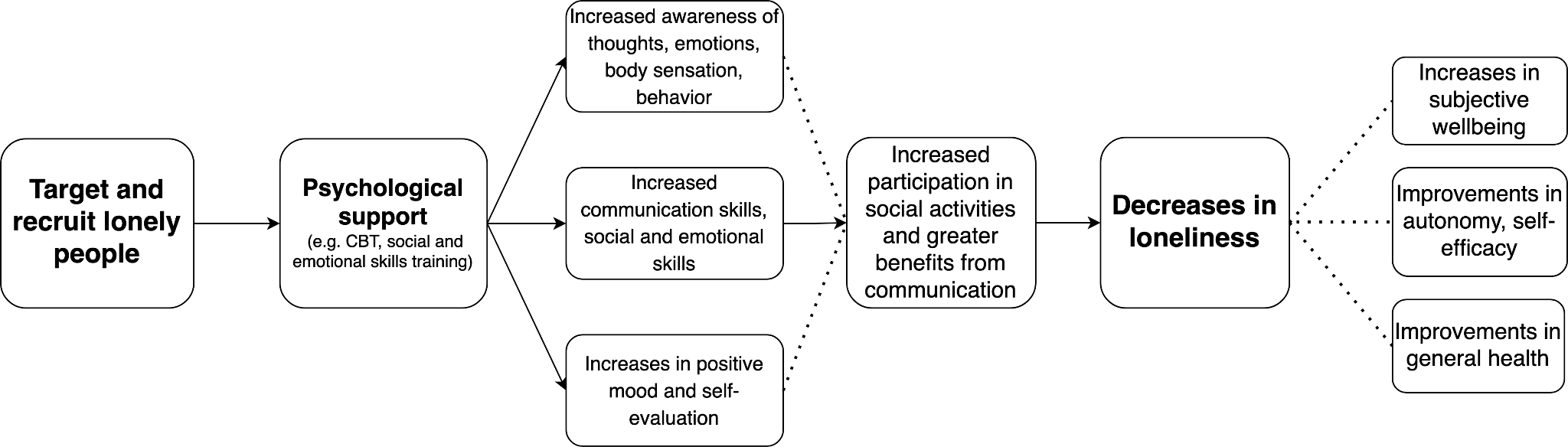
Befriending: A potential theory of change graph.[9]
Befriending interventions: some cost-efficiency data[10]
- In the Netherlands, providing a befriending service to recently bereaved widows and widowers (n=110 intervention, vs usual care n=106) was associated with a cost per 1 QALY gained = €6,827, median ICUR of €4,123 where primary outcome was a general health related quality of life status (via the EQ-5D scale). These estimates only include direct costs. When indirect costs are included the ICUR is estimated at €11,239. Intervention participants had significant improvements but the intervention arm did not differ significantly from the control group in their changes in health-related quality of life over time[11]. (Onrust et al., 2008)
- Importantly, Onrust and colleagues argue that befriending interventions for bereaved individuals will not produce large benefits for public mental health when targeted towards the entire population of all widowed individuals. They anticipate that widowed individuals will, over time, adapt and adjust and will not require a specific intervention to reach pre-bereavement levels of functioning. Moreover, they do not make frequent use of health care services related to bereavement. This is supported by additional research (Schut et al., 2001; Jordan & Neimeyer, 2011). A possible recommendation is to identify those who most benefit and need this type of intervention. It is also crucial to distinguish between general health or mental health needs and functioning versus needs for social opportunities and loneliness (directly measured).
- In the UK, carers for people with dementia (n=116 intervention, n=120 control) were offered a befriending service from trained lay workers and evaluated for quality of life and psychological well-being. There was no evidence for effectiveness nor cost-effectiveness. This intervention was linked to a cost per 1 QALY gained = £105,954. Further, there was no significant difference between intervention and control arms (RCT, Charlesworth et al, 2008).
- Bauer, Knapp and Perkins aimed to model the cost-effectiveness of the UK’s NHS running a befriending intervention, targeting lonely and socially isolated adults over 50, specifically by providing home visits for an hour per week for 12 weeks compared to usual care. Their model looked at reduction in depressive symptoms and reduction in use of health services as outcomes. This intervention was not cost saving over a 1-year time frame, as for every £85 invested (lower-end public cost of providing befriending) the NHS saved around £40 (Bauer, Knapp, & Perkins, 2011; section 2.15). The authors suggested that overall ‘befriending interventions are unlikely to achieve cost savings to the public purse, but they do improve an individual’s quality of life at a low cost.’ Further, when quality of life benefits associated with reduced depressive symptoms were included in a separate model, the authors suggested these interventions might be more cost-effective with an ICER of around £2,900.
- A friendship program involving older women (>55 years; mean age 63, sample size: 60 intervention, 55 control) with 12 weekly lessons on social topics (e.g. friendship, self-esteem; same intervention model as the ‘Friendship Enrichment Programme’) had significant positive effects on self-reported number of friends, self-esteem, life satisfaction, and loneliness for the intervention participants. Importantly, differences between the intervention group and control for loneliness was not significant (loneliness decreased by 4% in the intervention arm vs 3% for control, this wasn’t statistically different). It cost £77 per person at baseline and £120 per person including follow-up, and estimates a savings of £391 per person, and a gain of .035 QALY per person. (Optimity Matrix review for NICE, 2015; Martina & Stevens, 2006)
- This programme has also been probabilistically evaluated in Australia (Friendship Enrichment Programme, see Engel et al., 2021), where similarly modeling indicated the programme to be cost saving and, under some but not all probabilistic analyses, potentially cost-effective from a public health perspective (under A$50,000 per QALY gained).
Addressing barriers: How can befriending interventions be improved?
- Less demanding and lower cost training requirements for staff (see Richards & Sucklin 2009)
- Telephone or video-based systems (see Richards & Sucklin 2009)
- Evidence on peer befriending is limited but it could be a promising avenue to explore
- Hardly any evidence on befriending in LMICs and little on lonely young people
- Longer duration befriending interventions may be more effective and more wanted
Participation in social and healthy lifestyle activities
In these interventions, an activity is provided that aims to bring people together. These can be purely social or otherwise target healthy lifestyles, provide training or education.
One qualitative review found 9 group interventions involving the provision of an educational service (Cattan et al. 2005). 5 of these interventions demonstrated a significant reduction in loneliness and 4 did not. Participants did not seem to be recruited on the basis of baseline loneliness (but rather e.g. recruited via media campaigns or all eligible patients on GP lists). A systematic review examining interventions for loneliness for adults living in long term-care facilities found support for the effectiveness that provide opportunities for social bonding and group activities, such as horticultural therapy and laughter therapy (Guan et al., 2019).
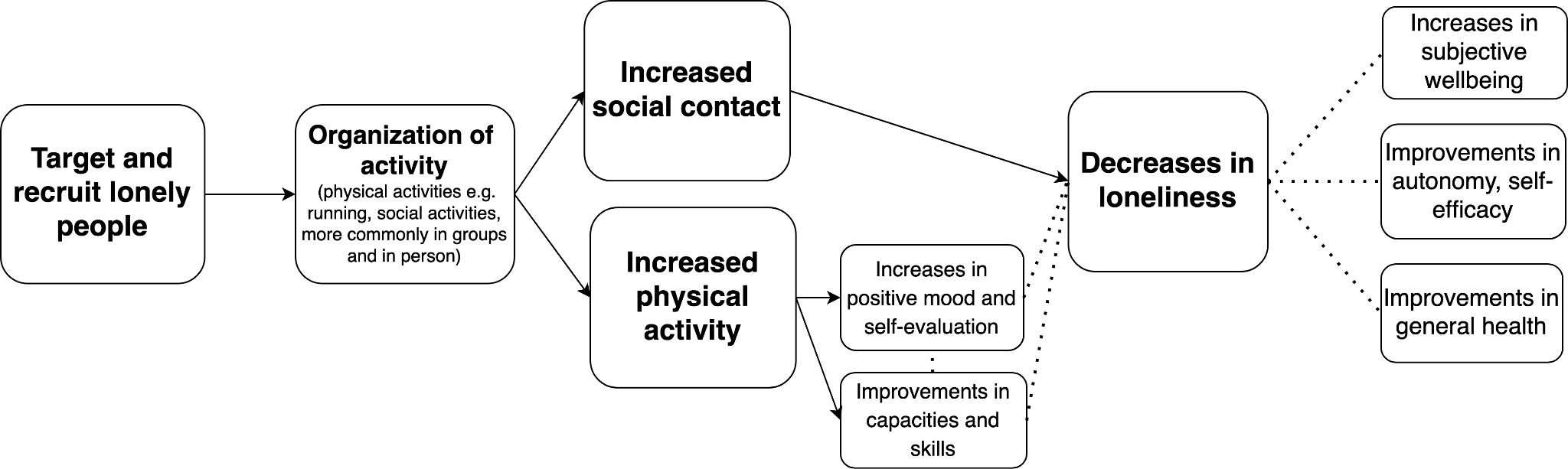
Participation in activities as a loneliness interventions: A potential theory of change graph.
Social & healthy lifestyle interventions: some cost-efficiency data
- ‘GoodGyms’[12] is an intergenerational intervention bringing together old and young runners. Here, 1 QALY gained = £8000, likely that there’s a return on every £1 invested of up to £4.56 (only considering at health and economic benefits; Ecorys UK)
- An arts-based intervention in the USA involving 30-weeks of chorale singing was narrowly cost saving, with a running cost of £86 per person and an estimated yield of health system savings of £92 per person. (Optimity Matrix review for NICE, 2015)
- An internet and computer training program (e.g. use of email, Internet) for older people was linked to costs of £564 per person and had an ICER of £15,962 per QALY gained. Importantly, this intervention did not have a statistically significant impact on participants’ loneliness and depression. (Optimity Matrix review for NICE, 2015)
Addressing barriers: How can social & healthy lifestyle interventions be improved?
- Group social interventions seem more effective than 1-1 interventions and so group interventions should be given priority consideration when feasible (Cattan and colleagues 2005)
- Targeting of those experiencing loneliness is not common and is a key problem
- There is evidence to suggest more specific targeting (e.g. care-givers, recently widowed people, physically inactive people etc.) and provision of appropriate, relevant services is associated with better outcomes[13] (Cattan and colleagues 2005)
Signposting/ navigation services
These interventions generally do not provide a direct or frequent service but rather refer people to service or appropriate resources. Evidence is somewhat scarce and largely hails from observational studies.
Cattan and colleagues (2005) found 4 interventions that provided health assessments with information services. 3 large-scale RCTs were not effective in reducing loneliness and 1 study seemed promising in that a one-off home visit by a nurse to provide advice, referrals and written health information demonstrated a significant reduction in loneliness but this effect wore off soon after the visit.
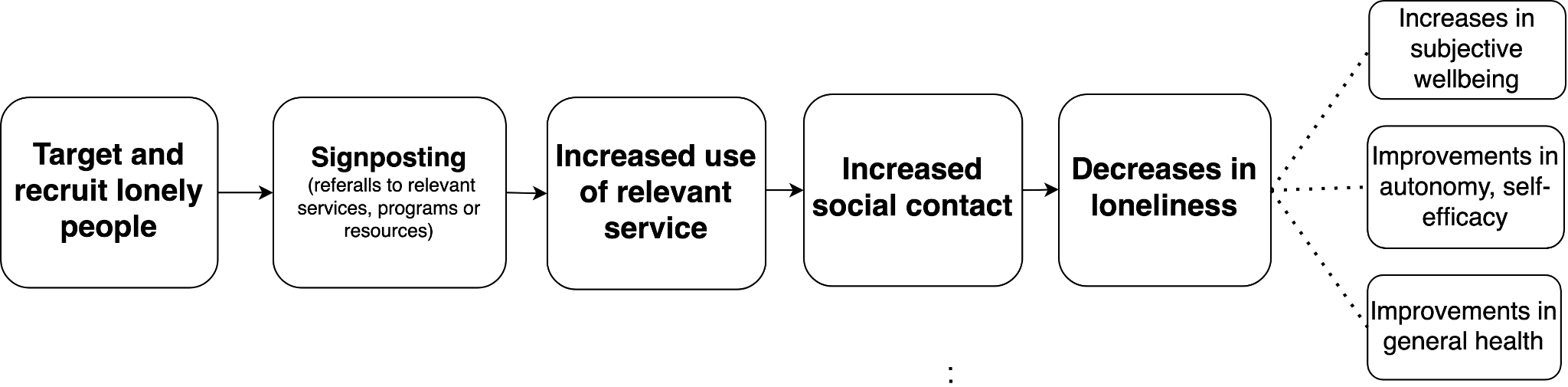
Signposting as a loneliness intervention : A potential theory of change graph.
Signposting interventions: some cost-efficiency data
- McDaid, Park, & Knapp, 2017 find a positive but small return on investment from a signposting to various activities: for every £1 invested, £1.26 returned (only looking at benefits to mental health) so could go up to £2-3 saved per pound invested.
- It seems most of these services don’t successfully target people experiencing more severe levels of loneliness
Addressing barriers: How can signposting interventions be improved?
- Better targeting is essential but given the existing evidence base it is unclear if that alone will make this stream of interventions effective.
- At present, it may be more appropriate to support interventions providing direct services.
Psychological interventions
Psychological interventions, such as CBT or provision of social skills training, seem cautiously effective in reducing loneliness. While Hickin et al. (2021) find an overall medium effect size (g = 0.43) this is based on a relatively low (k = 28 studies but only n = 3039 for the meta-analysis) and very heterogeneous sample (e.g. all ages, with and without other health problems). Notably some of the included studies have no follow-up or only a short follow-up. The causal mechanism is unclear. I speculate that psychosocial therapy likely improves self regulation, mood and may help provide social skills for people who need them but equally, since these interventions are delivered in social contexts (in groups or 1-1 with therapist or trained practitioner) they also provide social contact which may (temporarily) reduce loneliness (rather than the psychological component of the intervention).[14] It seems that provision of psychosocial therapies (which can be costly due to training and costing of time for clinicians) should be more carefully considered and a relevance profile for the targeted population should be established first. For instance, it appears inappropriate to offer psychological service to socially isolated people whose core need is social contact and who do not otherwise have problems with social skills or psychological problems.
Where might such services be most effective and warranted? One meta-analysis (Eccles & Qualter, 2021) examining loneliness alleviation in young people provides evidence for the effectiveness of a variety of interventions under this umbrella, including social skills training, social + emotional skills training, and psychological interventions (with no significant differences between intervention types, effect sizes varying around g=.262 to .350). This should still be taken with caution as most youth were recruited as they were considered to be at risk for e.g. health conditions, and were not targeted because of their reported loneliness. It is also unclear whether any reported levels of loneliness spoke to transient or chronic states. Future work should provide better targeting and measurement. Nevertheless, as adolescence is a particularly important period where social skills are still developing, these interventions might be particularly suited for this age group and may potentially become more cost-effective with better targeting. I note as well that included studies in this review involved young people living with physical health problems (e.g. HIV; cerebral palsy) but some of these interventions targeted young people or children with mental health or behavioral or developmental disorders, for instance autism, social anxiety disorder, behavioral disorders, and complex communication needs (e.g. as a result of physical disability). Outside of this age range, more careful consideration about social skills need and support are warranted to provide appropriate interventions, which likely include psychological interventions.
A ‘happiness’ intervention: cost-efficiency data
- In the Netherlands, a randomized single blind trial targeted people who experienced loneliness, health problems and reported low socioeconomic status (n=58 intervention, 50 control). The intervention “Happiness Route” provided home visits by a counselor who offered a happiness based approach in the intervention arm. The primary outcome was wellbeing but there were no significant improvements over time. The researchers estimated that expected costs per 1 QALY was €219,948 in the Happiness Route relative to control (Weiss et al., 2020).
Addressing barriers: How can psychological interventions be improved?
- More careful consideration of the needs of the population targeted (e.g. age, existing mental health problems or current communication skills).
- Considering attrition is relevant, particularly as there is some evidence to suggest that patients with depression are most likely to drop out of CBT (Fernandez et al., 2015). Further support may be warranted for some, according to risk profile.
- Providing CBT or other clinical therapies can be costly (e.g. therapist training, time) so this should be carefully offered. Alternatives like trained volunteers should be considered, as these seem promising in other contexts.
Intergenerational cohabitation
Intergenerational cohabitation was popularized by American activist Maggie Kuhn, founder of the Gray Panthers (1970), who championed the rights of the elderly. This idea later spread to the UK and Spain around the 1980. These interventions appear theoretically promising and may function similarly to befriending interventions provided over longer periods of time, thus permitting for closer and more sustained relationships.
Despite 50 years of interest, high-quality evidence (systematic reviews, RCTs, longitudinal studies) regarding intergenerational living programmes, where younger and older people live together, and their potential effect on loneliness is missing. In Australia, there is qualitative evidence that intergenerational living was a positive experience and intergenerational relationships were meaningful (Gurung et al., 2022). The WeShareWeCare project in France, Belgium, Spain and the United Kingdom offered a feasibility review suggesting intergenerational programs could suit matching elderly and international students moving to study in a foreign country under a variety of practical arrangements (such as free or reduced fee home sharing among others). In Alicante, a municipal project for intergenerational housing and community service provided qualitative evidence for improvements in wellbeing, while maintaining independence and offering increased social contact.
At present, a promising next step for funders and researchers could be collaborating with charities (e.g. Share and Care Homeshare, Helpful Housemates, United for All Ages, Intergenerational Housing Network, see further in the Intergenerational Housing Blog) and relevant (current or potential) direct service providers, including relevant stakeholders at local governmental levels to establish an evidence base.
Notes on neglectedness[15]
Funders
It is difficult to say who the biggest funders are in the field as funding seems distributed across a variety of sources with different levels of transparency and frequency of reporting.
A lot of funding seems to come from high-income countries including the UK, America, Canada, Australia, and some European countries and seems to primarily target within-country efforts, though there are global efforts as well. The UK seems to be the global leader in terms of funding.
International organizations such as the WHO and the UN have also been involved in this field but funding amounts and key priorities are unclear. The WHO’s team on Social Determinants of Health, particularly the unit for Demographic Change and Healthy Ageing has a focus on social isolation and loneliness. The most relevant branch within the UN appears to be the Department of Economic and Social Affairs (UNDESA) and their programme on ageing. WHO, DESA, ITU and UN Women have also launched an advocacy brief on social isolation and loneliness in older people (2021).
Some of the specific organizations that have been involved in funding and implementation programs to combat loneliness include:
- the AARP Foundation (USA)
- the National Institutes of Health (NIH) (USA)
- the Co-op Foundation (UK)
- and Age UK (UK)
- the British Red Cross (UK)
- the Campaign to End Loneliness (UK)
In 2018 the UK government announced a £20 million fund for projects tackling loneliness, of which £11.5 were provided from the Government, the Big Lottery, and the Co-op. The rest of the amount was provided by the Health Lottery and the Postcode Lottery. The annual Loneliness Engagement Fund will likely run again. It offers small grants between £15,000 and £50,000 to organizations who can engage with target groups at high risk of loneliness. Last year the fund spent £263,500.
NGOs
On NGO explorer, I find 57 NGOs[16] under the filter for ‘loneliness’, linked to a total spend of £756.5 million in 103 countries. Some of the biggest (by income) NGOs are presented below. Not all of these tackle loneliness as a primary aim. Note these are NGOs based in the UK (even if operating abroad), so the catch area for NGO Explorer is limited and will exclude charities e.g. based in the States (for example, Men’s Shed in the US).
| Organization | Profile | Latest income | Intervention or services |
| Age UK | Makes grants
Work in Bangladesh, Colombia, Ethiopia, Haiti, India, Jordan, Kenya and others | £127, 055, 000 (March 2021) | “Age UK aims to create a world where older people can live their lives free from poverty, isolation and neglect. It raises awareness of issues affecting older people in the UK and overseas, researches and campaigns for changes in policy and practice, and offers practical support to disadvantaged older people. It is funded by individuals, companies and trusts. “ |
| The Children’s Cancer and Leukaemia Group | Makes grants
Work in Ireland | £3, 890, 756 (December 2020) | “We fund and support innovative world-class research and collaborate, both nationally and internationally, to drive forward improvements in childhood cancer. Our award-winning information resources help lessen the anxiety, stress and loneliness commonly felt by families, giving support throughout the cancer journey.” |
| The Silver Line Helpline | Work in Guernsey, Isle of Man, and Jersey | £ 2, 599, 541 (March 2021) | “The Silver Line is a unique national service that provides three key functions to support older people:1. a signposting service to link them into the many and varied services that exist around the country;2. a friendship service to combat loneliness; and 3. a means of empowering those who may be suffering abuse and neglect and, if appropriate, transferring them to specialist services.” |
| My Israel | Makes grants
Work in Israel | £575, 404 (December 2020) | “Myisrael was founded in 2008 to support under-the-radar causes in Israel. Our causes cover mental health, special needs, poverty, homelessness, loneliness and education.” |
| Warm Hut UK | Work in England, Congo, France, Guinea, Côte d’Ivoire and | £275,577 (March 2021) | “Our mission is that African people gain a better insight into their experiences of living abroad, have a positive attitude towards life in the UK, maximise their well-being, feel empowered and enabled to contribute to the host country.” |
| Linking Lives | Work in Guernsey | £116, 642 (March 2021) | “Linking Lives UK is a national charity working to reduce lonelinessand social isolation amongst older people. We achieve this through the development of befriending schemes and social events and activities which are set up in partnership with local churches and other agencies. “ |
Conclusions
Summary of key points
- While loneliness is linked to a huge health and economic burden, more needs to be done to find robustly effective and cost-effective interventions.
- Evidence from meta-analyses shows there are different available interventions that can be effective to decrease the burden of loneliness. This is constrained by poor population targeting and short follow-up times.
- At the same time, not all loneliness interventions are effective. From the interventions this report found that are effective, only some are cost-saving, and fewer still are cost-effective from a public policy or government perspective (e.g. NHS: £20,000 - £30,000 per QALY gained).
- Understanding what works and which interventions types are most promising is not straightforward given methodological concerns and pronounced heterogeneity in population samples.
- Some key concerns include:
- Many interventions do not specifically target lonely people.
- Lack of longitudinal data.
- Difficulty to parse out causal mechanisms.
- Few are carried out in LMICs and we know little about the burden or loneliness there.
- Some theoretically promising interventions, like intergenerational living programs, are not robustly empirically evaluated.
What’s next?
Future opportunities for research
- Transparency and theoretical justification for definitions used for loneliness (e.g. see Prohaska et al., 2020; Surkalim et al., 2022)
- Improvements in measurement, including transparency in reporting, synchrony, comparability (e.g see Nicolaisen & Thorsen, 2014; Surkalim et al., 2022)
- Careful consideration between single item measures (commonly directly asking about ‘loneliness’ and scales (that commonly exclude direct mention of ‘loneliness’)
- Use of both direct and indirect measures when possible
- Promoting use of validated loneliness measures in global health surveys
- Addressing the lack of longitudinal studies in order to better understand loneliness over the lifespan (Surkalim et al., 2022)
- Improvements in methodology including repeated measures, and more common reporting of prevalence, including confidence intervals (Surkalim et al., 2022)
- Addressing the lack of longitudinal and prevalence data, as well as interventional work in LMICs
- Application of health approaches, broader consideration of individual risk profiles and social determinants, consideration of loneliness as a multidimensional construct (Akhter-Khan & Au, 2020)
- Better leveraging or further developing international research collaborations such as I-LINK
- Working with focus groups to better understand needs and examine if novel types of interventions may be more promising
Future opportunities for charity entrepreneurship
- Better targeting will improve our understanding of cost-effectiveness, so careful consideration of high risk groups is warranted, such as for instance recently widowed elderly people.
- Careful analysis of costs and ways to decrease them, e.g. particularly training costs and remote services
- Intervening early may also be cost effective, as current modeling suggests more of the economic burden of being chronically lonely may be experienced early on (Fulton & Jupp, 2015).
- Supporting and/or developing interventions with clear theory of change (for instance, happiness promoting interventions may be inappropriate when core need/deficit is lack of social opportunities)
- Evaluating existing efforts by charities, especially where there are gaps in evidence, such as for intergenerational housing
- “Simplify and scale” model
Notes
This shallow investigation is part of the Cause Innovation Bootcamp, please do watch out for future iterations of it. My thanks firstly go out to the organizers, Leonie Falk and Akhil Bansal. Special thanks to Leonie for mentorship, guidance, and feedback. Thank you to Aisling Leow and Eva-Lotta Käsper for further feedback. All errors are my own.
[1] There are claims from academics and activists in the field suggesting that loneliness has a comparable impact on mortality as smoking 15 cigarettes per day and that it is twice as unhealthy as obesity. These estimates have been used to make the point that while there are campaigns to address loneliness in Western countries, efforts are still lagging behind, especially when compared to similar or ‘less’ impactful health problems that have drawn very wide media and policy attention. With this in mind, it’s possible to have a higher estimate for neglectedness. At present I am somewhat skeptical about these comparisons due to the opaque nature of some survey designs and methodological choices.
[2] A note to illustrate different mechanisms and varying evidence. One systematic review (k=33) broadly suggests loneliness acts as a biopsychosocial stressor (Pettite et al., 2015). For instance, there seems to be good and varied evidence (covering biological and survey data) indicating loneliness as a risk factor for cardiovascular problems such as hypertension, coronary heart disease, heart failure, ischemic stroke among others. (Pettite et al., 2015). One systematic review of prospective longitudinal studies suggests that being lonely is associated with an increased risk of developing coronary heart disease and stroke of around 30% (Valtora et al., 2016). As a direct relationship, research has suggested lonely adults have greater activation of the sympathetic branch of the autonomic nervous system – this system activates body processes in times of stress or danger, providing the commonly known ‘fight or flight response’. Indirect effects are also possible, such as behaviors or cognitive patterns associated with loneliness, including negative self-appraisals, rumination and dissatisfaction, impacting other health behaviors (e.g. poor sleep or self-maintenance) that convey a risk for cardiovascular health. At the same time, some of the hypothesized impacts of loneliness are less well established and while plausible, merit more research. Such is the relationship between loneliness and malnutrition, which seems most pronounced for older people and where evidence tends to come from correlational, cross-sectional surveys (e.g. Eskelinen, Harikainen, Nykänen, 2016).
[3] For skepticism around the claim ‘loneliness is increasing’, see this blogpost from 2018 by Timothy Taylor.
[4] Because the authors were interested in problematic levels of loneliness this meant that they sometimes imposed cut-offs for the prevalence meta-analyses, such as a threshold of 5 or 6 on the de Jong Gierveld Loneliness Scale. This may be why their estimates point to lower prevalences rates than e.g. Campaign to End Loneliness whose prevalence percentages seem to include lower thresholds, i.e. occasional experience of loneliness. Even occasional experience of loneliness is associated with health risks, and so both types of estimates, representing different cut-offs for severity, are useful.
[5] Note these two estimates come from 2015 and 2020 and so are not immediately comparable.
[6] For the purposes of this shallow investigation, WELLBY calculations are based solely on this one report and two surveys. More robust estimates can likely be obtained with further data.
[7] I note I haven’t found descriptive statistics (e.g. n or proportions) for each level of loneliness.
[8] The ONS reports a total of 13 million for the categories ‘Some of the time’ and ‘Occasionally’ jointly, so my split into 4 & 9 million is somewhat arbitrary.
[9] All of my theory of change graphs have a degree of theoretical abstraction and may not apply with equal specificity to all interventions. Notably, most interventions I found did not actually recruit lonely people specifically.
[10] I provide summaries of already existing CEAs. One point of feedback I received is that cost-effectiveness estimates provided from the original interventions may underestimate cost. I’ve looked at the breakdowns of costs and at face value do not find this to be likely. Instead, I think it is more important to note that the interventions for which I was able to find computed CEAs may not be representative. It is possible that there are more cost-effective interventions. Nevertheless, I hope the provided estimates prove helpful for a further more rigorous look into the cost-effectiveness profile of different interventions tackling loneliness.
[11] I note intervention arm participants reported higher levels of loneliness at baseline, but even after adjusting for this, there were no significant differences between control and intervention arm.
[12] Arguably could also be considered a befriending or intergenerational intervention. I’ve listed it under the health activities interventions as I see additional potential benefits in this stream of work that otherwise are not typically provided in other services (e.g. befriending).
[13] Though this may also be because these interventions had better theories of change and more careful consideration of mechanisms from the beginning
[14] A related point is discussed in a systematic review Bessaha et al. (2020) examining a variety of interventions, where it was unclear whether the mechanism of an intervention was associated with change or the driver was providing social contact to people from the same groups (e.g. refugees, people with chronic illness)
[15] This section sketches funding in the area but does not cover other efforts such as awareness or media campaigns, activists efforts, or political work (e.g. Japan has a Minister in charge of Measures for Loneliness and Isolation).
[16] NB not all provide direct services relating to loneliness but may be picked up by this filter if they mention something around this term.

I appreciate this post! Loneliness is something I think about often because it appears to be, alongside mental health issues, as one of the things that appears relatively worse for people's subjective wellbeing than say, their income.
That being said, it was always unclear what can be done, and this review doesn't seem to suggest there's a frontrunner in terms of interventions.
A question I'm curious about is what are the biggest barriers to lonely people going out and making friends on their own? Is it transportation? Cost? Unclear where to go? Church used to be the easy button, but many people aren't religious anymore and we don't have a clear substitute. Why isn't this a problem that markets can solve?
What about digital interventions? Some people seem to be content with forming and maintaining relationships through a digital medium (e.g., online gaming).
I'd also really like to know how common loneliness is in low income countries, and how the barriers differ towards forming more positive social bonds.
I'm equally curious about all the questions you raise. I briefly skimmed this paper, which seems to have a few interesting points in reference to succesful intervention methods:
In response to your question of:
The answer seems to be that extreme loneliness may be based on having a poor social environment, where loneliness no longer becomes a motivating factor to just go out and socialize, but instead isolate?
This 2nd paper concludes:
This all seems to suggest that building programs to adjust social patterns may be the most effective form of preventing/reducing loneliness. It strikes me that this form of intervention would likely be expensive if done 1-1 (as it'd most likely be done through trained therapists, which are quite expensive), but possibly could be done en masse for cheap? Possibly a website or app to intake symptoms and suggest changes to one's behavior could be somewhat effective? [Reducing CBT to an app/AI platform seems to currently be failing.] (https://www.nytimes.com/2021/06/01/health/artificial-intelligence-therapy-woebot.html)
I have no education/experience in analyzing psychological papers though, so hopefully someone with more experience can chime in and let me know if my 10-minute skim and analysis is incorrect.
Thanks very much for writing this up! I thought it was very interesting, and appreciate all the work you did.
This seems like a pretty common view, and I've come across other pieces of evidence about the adverse impacts of retirement on a lot of people. I wonder if a positive step would be to raise the retirement age? Clearly this is a massive policy change, so would do poorly on tractability, except that it's one that a lot of people support for other reasons (e.g. improving dependency ratios, GDP growth).
The other thing that seems like it could help here is encouraging and removing barriers to people having more children. Anecdotally, children and grandchildren seem to form an increasing fraction of people's social network as they age because they attrition much slower than friends or colleagues (assuming you're not a terrible parent); I think a lot of young people underestimate how big of a difference 3 children + 9 grandchildren would make vs 1 child and 1 grandchild. Like the above, it's a massive policy issue, but one where there are many other reasons to support it, which could improve the marginal tractability.
This sounds plausible. I wonder if people's attitudes towards retirement is a huge affective forecasting error where they think it'll be sublime, but it ends up isolating and boring (like school breaks were for me as a kid).
But I wonder if that attrition isn't related to parenthood. I haven't had kids yet but my friends seem to drop off the map socially as they become parents. It's sort of concerning. Having children also seems pretty isolating to many living in environments that cater to nuclear families.
Surely there's evidence for this question as it pertains to loneliness. I know that having grandchildren is clearly good for subjective wellbeing, but the evidence for the effects of parenthood, in general, are much more mixed/ambiguous.
If raising the retirement age is not feasible, another option might be to create more and better opportunities for retired people to engage with and contribute to society in part-time paid or volunteer work?
My impression is that here in Germany, it seems like the potential of retired people might still be underused (based on very anecdotal evidence, I didn't research this).
In Sweden, at least among the middle classes, it's not unusual to hire seniors for odd jobs (it's cheaper, you pay less taxes), e.g. via services like this one. It's kind of a win-win situation: one party gets to hire someone for pretty cheap to get something done (e.g. some garden work or handiwork -- I'm guessing quite often things they wouldn't have paid anyone to do otherwise), and the other gets some extra money, human interactions and the satisfaction of non-backbreaking manual labour.
I didn’t read this, but my very first foray into “doing good” was building a web app to fight loneliness via helping people make friends online (2010-2013).
We didn’t get to see what it could become as I became passionate about doing other EA things (joined CEA then) but I’ve sometimes wondered if continuing with that app would have been the right call. I think there’s some chance we had found the right design / product for this space.
Anyway if anyone feels like picking up the codebase or otherwise trying to move forward with a massive loneliness intervention, I’d be open to messaging about it.
By chance have you considered/investigated AI friends?
My impression is that they could be a really big deal. Possibly really net-bad, possibly really net-good.
https://www.facebook.com/ozzie.gooen/posts/pfbid0mRoPn5o3hdEAjzryhZQ7sTAR6EXLwTjhPPrGUrVHft65u75WmgmisiGVo3qtwNPCl
I'm specifically hopeful about this cause area because
I'm confused about why this wasn't solved yet. Is it just hard to monitize? I don't know
Something important seems missing from this approach.
I see many hints that much of this loneliness results from trade-offs made by modern Western culture, neglecting (or repressing) tightly-knit local community ties to achieve other valuable goals.
My sources for these hints are these books:
One point from WEIRDest People is summarized here:
Can Western culture give lower priority to independence while retaining most of the benefits of WEIRD culture?
Should we expect to do much about loneliness without something along those lines?
AI seems likely to have some impact on loneliness. Can we predict and speed up the good impacts?
Most Westerners underestimate the importance of avoiding loneliness. But I'm confused as to how we should do something about that.
I think this is a very thorough and interesting post. I think the post focuses mostly on interventions to directly treat social anxious people, as we would treat people for other mental health problems. While I think researching and implementing these treatments is worthwhile, I also think that we want to pursue solutions to the underlying technological and cultural shifts that may have caused the significant upswing in loneliness in past decades. Below I'll share the contents of an essay I recently wrote about about some potential solutions. I'd be curious to hear what thoughts other readers have about these potential solutions. I apologize in advance for the unsettling AI art :) I wanted to find a way to quickly get images for the essay without having to worry about copyright, so I used ChatGPT.
4 Ways to Solve Our Loneliness Crisis
The Problem
Many articles have established that loneliness is a significant and growing problem facing America, so I won’t spend too much time establishing the importance of the issue.
In May 2023, the US Surgeon General Vivek Murthy released an Advisory calling attention to the public health crisis of loneliness, highlighting how loneliness is bad for physical and mental health: “Loneliness is far more than just a bad feeling — it harms both individual and societal health. It is associated with a greater risk of cardiovascular disease, dementia, stroke, depression, anxiety, and premature death. The mortality impact of being socially disconnected is similar to that caused by smoking up to 15 cigarettes a day.” Murthy also explained that loneliness is prevalent and on the rise: “Changes in key indicators, including individual social participation, demographics, community involvement, and use of technology over time, suggest both overall societal declines in social connection and that, currently, a significant portion of Americans lack adequate social connection.”
Solutions
1. Restrict Smartphone Usage among Kids
Smartphones and especially social media, have been thought to be harmful to the social lives of kids. According to a NY Times article written by psychologists Jonathan Haidt and Jean M. Twenge: “In a paper we just published in The Journal of Adolescence, we report that in 36 out of 37 countries, loneliness at school has increased since 2012. . .This synchronized global increase in teenage loneliness suggests a global cause, and the timing is right for smartphones and social media to be major contributors.” The authors go on to say that after examining a number of global trends that might explain the rise of teenage loneliness, only smartphone use and internet access appeared to move in lockstep with teen loneliness.
The two psychologists recommend the following solutions: ban smartphones in schools and delay entry to social media via effective age gating. With no smartphones in school, students can practice “the lost art of paying full attention to the people around them.”
Social media, which has been thought to be the most deleterious form of smartphone uses, especially for teenage girls, can be restricted by effective age gating. Tech platforms have nominally age gated their platforms, but teens can easily bypass these mechanisms by lying about their age. Although I generally pride myself in being honest, I remember lying myself to gain access to Facebook in middle school. According to the article tech platforms “should be required to implement age and identity verification for all new accounts, as many other industries have done. . . the verification could be done by reliable third parties.” States have actually begun passing laws to enforce age gating and restricting the use of social media apps for minors. In spring 2023, Utah passed laws imposing a curfew on social media use for minors, making their sites off limits between the hours of 10:30 p.m. — 6:30 a.m. for anyone under the age of 18. The laws also seek to curtail tech companies ability to lure kids to their apps using addictive features. Utah is the first state to enact such laws, but other states such as Arkansas, Texas, Ohio, Louisiana and New Jersey have similar proposals in the works.
We can contact our local schools and state representatives to help promote school phone bans and effective age gating of social media platforms.
2. Facilitate More Unsupervised Play
Jonathan Haidt argues that there has been a significant reduction in unsupervised play among kids in America for many decades. Unsupervised play is essentially play that is freely chosen by kids and not overseen by adults. Haidt believes that less unsupervised play for kids means a whole host of harms, including weaker social skill development. I speculate that the reduction in unsupervised play has been a major factor in loneliness of both kids and adults (who developed weaker social skills as kids).
Why did unsupervised play decrease? Haidt argues that a major cause of the decline was an irrational fears of kids being abducted that arose in the last 20th century. The data shows that there was never much risk of child abduction. But television portrayed heinous abductions, making parents afraid to let their kids play freely. Eventually, new social norms of kids needing constant supervision were reinforced by state negligence laws making it illegal for parents to let their kids roam unsupervised in many places. Haidt also pointed out that Kids spend an increasing amount of time doing homework and supervised activities like sports outside school, crowding out time for unsupervised play.
How can we increase the amount of unsupervised play our kids have? We can potentially educate parents on the safety and health benefits of allowing their kids to engage in unsupervised play via the media or existing parental education programs. We can contact our state legislatures to advocate for changing negligence laws to be more permissive of unsupervised play. We can work with our local schools to reduce the amount of hours of homework children have.
We can get involved in our local zoning boards to stop new housing projects from being blocked, allowing for more dense and walkable communities. We can ask our representatives to fund better public transit. With denser housing development and improved transit, more kids will likely live in neighborhoods where they can reach their friends’ homes without being dependent on parents’ car rides (which can be limited in supply).
3. Leverage Economies of Scale in Parenting
In this section, I’ll offer a solution that may improve the social lives of parents. Let me preface this section by acknowledging that I have no personal experience parenting. I hope to be a parent one day and I am daunted by the sacrifice and stress that parenting appears to require.
Anecdotally, I have several single friends in their 30s and I hear from them that most of their friends have kids and are hardly ever free to hangout. According to an article by the World Economic Forum, from the American Time Use Survey “When we’re young — particularly in our teens — we spend a lot of our time with friends, parents, siblings and extended family. . . Throughout our 30s, 40s and 50s — over this period of [our] life, [we] spend much of their time with partners, children and, unsurprisingly, co-workers.” The article goes on to say that for adults with children, the fraction of their time spent with people outside their immediate family is even less than the average for adults. In sum, parents’ friendships and social lives outside their immediate family typically weaken significantly.
Is having a limited social life outside one’s immediate family an inevitable cost of parenting? According to Kristen Ghodsee, a professor at the University of Pennsylvania, this needn’t be the case. In her book, Everyday Utopia, Ghodsee discusses how throughout history, people have relied on larger networks beyond the nuclear family to assist with parenting — extended family, neighbors, and fellow community members. American parenting culture, where almost all the effort of raising children falls on the nuclear family, is a fairly unique division of labor. Ghodsee suggests that Americans should strive to leverage extended networks to help reduce the heavy burden of parenting. Americans should consider living closer to their extended family members and seeking help from family. For example parents could have grandparents help watch children. Friends who are raising children could move in together or buy nearby units, helping take turns watching each other’s children or cooking meals (see this podcast episode for a real life example).
While searching Google, I came across a medium post by environmental engineer Katie Patrick, proposing a coliving unit design for parents to efficiently raise children together. The residence could consist of a bunch of studio apartments adjoining a central play space. According to Patrick, the space could have a “A roster of parent rotation to cook dinner and oversee the children from 5pm — 10pm. Each parent is on duty about 2 to 4 nights per month. . . Parents are able to leave their child in the home from 5pm — 10pm on evenings supervised by the parent on duty.” Such an arrangement could massively reduce the workload for parents, allowing them to maintain vibrant social lives, reducing the stress on spousal relationships and improving happiness.
As another solution to parental isolation, universal child care could be subsidized or provided for free by the state or federal government. This solution would also provide parents with more time to socialize. In her book Ghodsee states that children are a public good. American citizens benefit from Americans having more children, yet the cost of having kids is born on individual families. With the high stress of parenting and the rising costs of raising a family in the US due to rising housing, higher education costs, and healthcare, parenting is in many ways increasingly difficult. Maybe we should reduce the burden of parenting to incentivize having more kids with free or subsidized child care? Of course, among other downsides, providing childcare at this scale would be a huge taxpayer burden. The benefits would have to be weighed against the costs.
Finally, changing norms and laws to allow kids of a relatively young age to roam their communities and play unsupervised could reduce parental isolation by reducing the amount of time parents need to spend watching over their kids and giving them rides.
4. Screen-Minimal Coliving Communities
I believe screen based entertainment is at the core of our loneliness problem. Harvard sociologist Robert Putnam argued that the introduction of TV reduced Americans’ participation in civic institutions like church or service organizations, which ultimately damaged our trust in each other and in our democracy. However, data seems to show that TV did not reduce our amount of hours spent doing social activities.
According to data from the American Time Use Survey, the amount of hours Americans spent with their friends between 1970–2013 remained relatively constant. Then, after 2013 the time dropped precipitously. What happened? According to the Australian writer Joseph Friedman, the decrease can be explained by the rise of smartphones, tablets, high-speed internet and affordable laptops. Friedman says: “30 years ago, we still crowded around the television with our tribe. Today, we stream alone, hunched in a corner of the house watching TV on a phone or a laptop, while our partners and children do the same in their corners, alone”
How can we solve our screen-based entertainment problem? Having the government simply ban screen-based entertainment would seem to me to be a problematic precedent-setting overstep of government authority. Instead, a more tenable if farfetched solution could be for like-minded people to live together in coliving communities where time spent on screens is limited. According to an Australian coliving company “Coliving is a modern form of housing where residents share living space and a set of interests, values, and/or intentions.” Coliving communities could be established to encourage community and social connection, in part by limiting the isolating effects of screen-based entertainment. How could screen-based entertainment be limited? Internet access could be blocked by making the walls and/or windows of the building contain materials known to block cell signals and by installing no internet/TV cables in units.
Residents could still work modern jobs by working from their workplaces or in coworking spaces in the surrounding metro areas. To allow residents to function in our digital-driven modern societies, cell signals (but not data signals) could be provided in buildings so people could still send and receive calls and texts, using a similar technology to how NYC brought cell + data signals to the NYC subway. A small computer lab could be provided to allow adults a limited amount of access to computers per month (e.g. 10hr) to do such errands as online shopping or planning a trip. Like many modern day coliving spaces, these communities could build social connection through regular community events (e.g. service activities, dinners, etc.), shared spaces (e.g. sports fields and courts, common rooms with games, etc.), and chores.
Without the ability of residents to easily entertain themselves in isolation, I suspect residents would be much more likely to want to spend time with each other, both in and out of the coliving space. These communities could be built as resident owned, nonprofits, or for profit organizations. I suspect the biggest barrier to building these coliving spaces would be that the downsides of living in such communities are very clear (limited access to the screens) while the upsides are currently speculative (better social life and sense of community). Possibly, a prospective founder of one of these spaces could target a segment of people who are most eager to live in an environment with limited screen access (e.g. parents who follow a particular religious tradition) and build a screen-minimal coliving community for them. Eventually if this group has a very positive experience and data by unbiased third party researchers shows the superior social outcomes of this living arrangement, more widespread interest in these living spaces could arise.
I would like to hear what you agree and disagree with!
FWIW, I've been shopping around a "peer support group" (PSG) program pilot for the past year that I think will address depression, anxiety and lonliness. I've been talking to Roscoe from StrongMinds, who says they are planning a trial of a modified version of their current group interpersonal therapy (IPT-G) intervention. If anyone wants to talk further about this, please DM me. davecort@pm.me
I’m a little late to this discussion, but I first want to say thank you for this post! This is a topic I’ve been interested in of late and your post filled in a lot of gaps in my knowledge.
I see the potential for this to be tractable for EA funders and entrepreneurs, because non-EA funders might be incentivized to fund the deployment of interventions that are effective enough. It’s unfortunate that lonely people are less healthy and less productive, in addition to having lower life-satisfaction, but this phenomenon may have a silver lining. There might be interventions that benefit lonely people, and that also provide enough benefit to their employers and/or insurers for those companies to be financially motivated to provide them. An intervention might not clear the EA bar for $/DALY or $/WELLBY, but if it provides a favorable return on investment for employers and insurers, it has the potential to be deployed at scale. An EA funder might still need to fund the development of the intervention, demonstration of its effectiveness, and the spreading of information about its effectiveness. And EA entrepreneurs would need to do the work.
There’s an organization called the Foundation for Social Connection that is funded by the Coalition to End Social Isolation. Two of the four members of the latter’s steering committee are large health insurers, and there are some large corporations among their members. The Foundation for Social Connection has an Innovation Accelerator that could be a good resource for organizations interested in this space. Some of the researchers cited in this post are affiliated with the organization.
In addition to employers and insurers, school districts are another possible funder for effective interventions. I know of a Social-Emotional Learning curriculum that aims to help students make “intentional connections.” Schools could potentially see short-term benefits that justify the cost (primarily the opportunity cost of classroom time) if the intervention improves students’ behavior, engagement, and well-being. Long-term benefits could be significant as well, but these would be more difficult to demonstrate.
One other thought: there might be benefit to thinking more broadly in terms of improving people’s relationships or connectedness, rather than just addressing loneliness. I would suspect that most people would benefit from some combination of (1) increased awareness of the importance of relationships for their physical health and emotional wellbeing; and (2) resources to help them improve their existing relationships and to form new high quality relationships.
I appreciate you formatting the post summary with brevity in mind :-) Makes it easy to quickly understand the main points and I can see you put in deliberate thought into formatting as a table.