In brief
Recently I became interested in what kind of costs were inflicted by iron deficiency, so I looked up studies until I got tired. This was not an exhaustive search, but the results are so striking that even with wide error bars I found them compelling. So compelling I wrote up a post with an algorithm for treating iron deficiency while minimizing the chance of poisoning yourself. I’ve put the algorithm and a summary of potential gains first to get your attention, but if you’re considering acting on this I strongly encourage you to continue reading to the rest of the post where I provide the evidence for my beliefs.
Tl;dr: If you are vegan or menstruate regularly, there’s a 10-50% chance you are iron deficient. Excess iron is dangerous so you shouldn’t supplement blindly, but deficiency is easy and cheap to diagnose with a common blood test. If you are deficient, iron supplementation is also easy and cheap and could give you a half standard deviation boost on multiple cognitive metrics (plus any exercise will be more effective). Due to the many uses of iron in the body, I expect moderate improvements in many areas, although how much and where will vary by person.
Note that I’m not a doctor and even if I was there isn’t good data on this, so it’s all pretty fuzzy. The following is an algorithm for treating iron deficiency that I’ve kludged together from various doctors. I strongly believe it is a lot better than nothing on average, but individuals vary a lot and you might be unlucky.
- Take a serum ferritin test. If you have a doctor they will almost certainly say yes to a request, or you can order for yourself at walkinlab.com
- If your results show a deficiency (<20ug/L), increase iron intake through diet or supplements such as Ferrochel, taking the default dose once per day, with a meal.
- The definition of deficiency can vary by study, lab and goal. I picked <20ug/L because it’s the highest level I have concrete evidence is insufficient, but personally believe people are likely to benefit from iron beyond that and am taking pills accordingly.
- If you experience negative effects after taking the pills, stop immediately. Give yourself a week to recover, then you can try other brands, be more careful to eat with a full meal, etc.
- If you are experiencing the symptoms of iron poisoning (listed below), stop pills and see a doctor now. Iron poisoning is a very big deal, which is why step 1 of this algorithm is “get tested” not “gobble pills”. Unfortunately several of these are pretty generic, but I’m never going to feel bad about telling people with seizures to seak medical attention:
- Nausea
- Vomiting
- Abdominal pain
- Dizziness
- Low blood pressure and a fast or weak pulse
- Headache
- Fever
- Shortness of breath and fluid in the lungs
- Grayish or bluish color in the skin
- Jaundice (yellowing of the skin due to liver damage)
- Seizures
- Black or bloody stools
- Retest at 8-12 weeks, ideally at the same lab as before.
- Continue to retest every 8-12 weeks.
- If you increase by 20ug from your starting value without noticing any improvements to your cognition or overall energy levels; low ferritin is probably not your bottleneck.
- If you believe it’s not a problem at all, quit.
- If you believe it is a problem but another problem is limiting your gains, stay on a maintenance dosage but don’t put more time into managing this. Verrrrry roughly, divide your current dosage by your currently monthly gains (so If you take one RDA/day and gain 10ug/month, your result is 0.1), and take that much. This hopefully keeps you from losing ground, without gaining so quickly it could become a problem.
- If you’re getting improvements, keep going until those taper off. I personally would exercise caution and investigate the downsides of iron once I reached 80ug/L, but I’ve never gotten close to that so it hasn’t come up.
- Continue to retest and adjust until you’ve found a dose on which your values are stable and healthy.
[Note: I provided links to supplements because I found people follow through more when I do, and because it’s easy to buy worthless supplements. There are other good supplements out there and if you have a reason to prefer one, take that instead. Links are affiliate.]
Research summary
Iron’s most famous use in the body is in hemoglobin, which your blood uses to transport oxygen. Oxygen is extremely important [citation needed], so it makes sense that low hemoglobin (aka anemia) gets a lot of attention, and everyone agrees anemia is very bad. But what the studies I read found was that even among people who started with adequate hemoglobin, a low ferritin score still predicted they would benefit from supplementation. And it’s not because of a bad definition of “adequate”; people saw benefits even when their hemoglobin didn’t change. So what else does iron do?
Iron is one of a small number of elements that can safely accept electrons in reduction-oxidation reactions. Free electrons are quite damaging, so iron’s ability to safely contain them is important. Some specific usages:
- The enzyme catalase, which converts caustic H2O2 to harmless water.
- Fun fact: Catalase is the least important enzyme whose name and purpose I can recall offhand. Other enzymes achieved that status by being very important (DNA polymerase), or having self explanatory names (carbohydrase), but catalase achieved this by sounding kind of similar to a song I was into the summer I took microbiology, and I made up alternate lyrics about the enzyme.
- Multiple points in DNA synthesis and repair, including keeping DNA polymerases in their correct shapes.
- Myoglobin: similar to hemoglobin it binds oxygen, but instead of blood it stays in muscles, holding oxygen in reserve until it is needed.
- Regulation of many components of the immune system.
- Proline and lysyl hydroxylases, both used to build collagen.
- Please enjoy this list of 80 enzymes that use iron as a cofactor.
I’d say “that’s a lot” but honestly it’s not, everything in the body is like this, it was not built to be understood.
Standard tests for anemia only look at hemoglobin. Ferritin tests are considered to be a much better measurement of cellular iron levels. There’s suspicion, although not proof, that your body prioritizes hemoglobin production above other uses of iron, so it will undersupply these other uses in order to maintain hemoglobin levels. This suggests that if you have normal hemoglobin but low ferritin, additional iron will find many uses. Unfortunately, those uses and their effects are so varied I can’t really predict what any particular person will experience.
There are any number of studies showing correlations between low ferritin and low functioning, but I don’t find those very useful. The people in those studies might have any number of deficiencies for multiple reasons, or low ferritin levels could just be a proxy for poverty. In my research I stuck to actual experiments, with controls, that gave iron to subjects and checked for an improvement in function, not just test scores. Unfortunately, there were not that many of them.
The only study I liked on the cognitive effects found an absolutely enormous effect. Successful iron supplementation led to improvements averaging >0.5 standard deviations in attention, learning, and memory. I have qualms about this study and expect the results are cherrypicked, but it’s also not necessarily the full size of the effect, because they stopped after a set amount of time rather than waiting for effects to plateau.
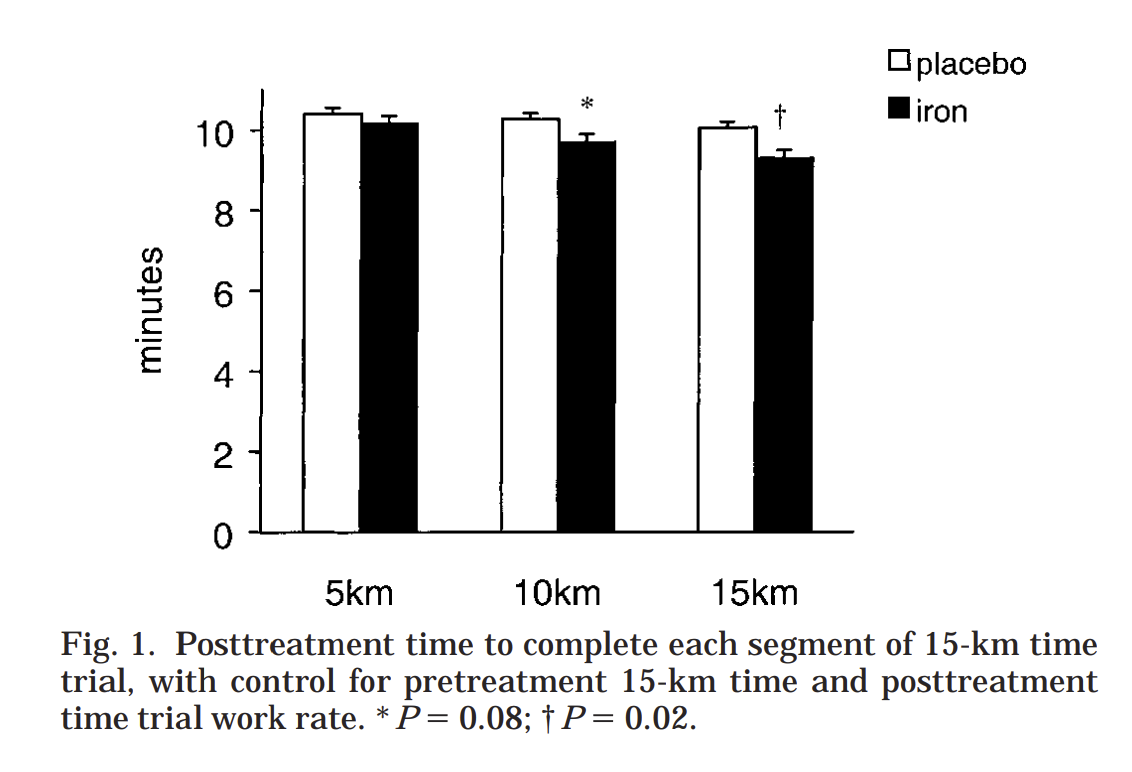
There were multiple studies on iron supplementation and exercise. In a nutshell: everyone’s endurance improves when they exercise. Giving people with iron deficiency but not anemia (IDNA) iron supplements increases that effect. In the strongest study, people treated for iron deficiency for 6 weeks improved their 15km time by 10%, compared to 5% in the control group. Another study (which didn’t involve exercise training) showed no improvement in time to complete a given distance, but did find the treatment group used about 5% less energy while doing so.
Iron deficiency rates vary a lot by population, but with the patterns you’d expect. Vegans are more deficient than vegetarians, who are more deficient than omnivores. People who regularly menstruate (or give blood) are more likely to be deficient. I found the baseline rate of omnivorous men in rich countries to be somewhere between 0-11%. For a female omnivore it’s 9-22% (these numbers include people already taking supplements; it’s presumably higher if you don’t). Young female vegans who were not already supplementing were at least 50% deficient, plausibly more. Data for non-supplementing male vegans was not available, but let’s ballpark it at 5-25%, based on the ratio between men and women in the general public.
People in poor countries are much more likely to be iron deficient and anemic, due to poor diet and more physical exertion.
Caveats
I am not a doctor, my most relevant credential is a BA in a different part of biology, the fact that I couldn’t find a decent resource and had to make it myself is a sign of civilizational inadequacy.
Normally not being a doctor inhibits me from giving medical advice, but I am going to go ahead and say that iron poisoning is extremely bad and not that hard to induce with pills, don’t do that. Iron poisoning is why you need to be careful your kid only gets one multivitamin a day, and why men can’t use women’s multivitamins (which should actually be “menstruator’s multivitamins”, since the relevant issue is monthly blood loss).
The papers are very finicky and boring and this was really important, so I’ve tried to frontload my conclusion. This is a delicate balancing act of readability and accuracy. I did my best but some trade-offs are unavoidable.
This lit review was done with a focus on people with low iron intake, especially vegans. None of the studies I looked at filtered on dietary intake versus absorption issues. This means they probably underestimate the impact of supplementing for healthy people.
Do not take the dosages in the studies literally, especially if you don’t menstruate. The right dosage depends on the form and your personal needs. I suggest operating based on RDA percentages rather than raw chemical weights.
Details
Definitions
There are a lot of ways to measure iron and iron-related levels in the body. The two most important are hemoglobin (the protein red blood cells use to carry oxygen) and ferritin (the protein your cells use to store oxygen, but also present in blood). There are some other numbers I’m going to ignore.
Hemoglobin and ferritin are both testable via blood sample, and the tests have something called “reference ranges”, which are supposed to be the healthy range of values. Whether the ranges actually capture that is a matter of great controversy, with various people alleging the minimum is what you need to avoid hardcore deficiency diseases, but won’t get you optimum functioning, to people claiming low scores are fine and anyone who says otherwise is a psyop from Big Vitamin. And then there’s individual variation.
Hemoglobin’s reference range is 120g/L-170g/L. Ferritin’s reference range starts between 10 and 20 ug/L, and ends at 150-200ug/L, depending on who you ask. It’s possible to have low hemoglobin (aka anemia) without an iron deficiency or vice versa. Low hemoglobin with adequate iron typically means you’re having trouble manufacturing hemoglobin and is beyond the scope of this post. Low iron with adequate hemoglobin is more controversial. Top explanations include “the tests aren’t that good”, “you’re deficient but your body is prioritizing hemoglobin production”, “you’re about to develop anemia” and “low iron is fine, actually”.
Impact Data
When looking at studies I used the following selection criteria:
- Examining iron deficiency without anemia. We can assume that anemic cases will benefit more from iron, unless the anemia is unrelated to the iron deficiency.
- No co-morbidities.
- On adult humans (in practice this almost always means women).
- In the developed world.
- RCTs only, no correlational studies.
This didn’t leave a lot of studies, and I had to accept some other flaws.
Mental
Murray-Kolb and Beard (2007)
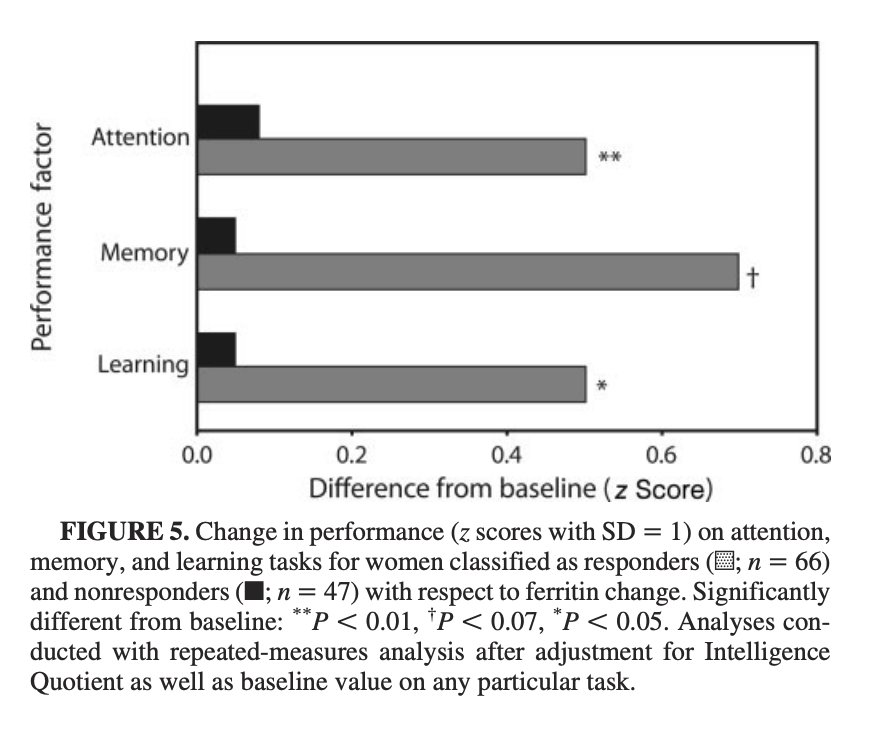
This study was by far the best study of cognitive function, maybe the only one that tested an intervention rather than merely looking at correlations. I don’t love it. The data presentation is obviously leaving a lot of information out, I assume to dramatize results. But those results are very dramatic.
This study allowed for mild anemia (hb < 120 but >105), but separated anemic and non-anemic subjects. The paper, uh, doesn’t mention its threshold for iron deficiency; another paper from the same authors set it at serum ferritin <=12ug/L, which is in line with the aggregated averages.
The study included a double control group that started with sufficient iron and hemoglobin. Each group (no deficiency (n=42), iron deficiency without anemia (n=73), and iron deficiency with anemia (n=34)) was split into treatment and placebo groups.
Iron supplementation increased ferritin levels in everyone. People with iron deficiency without anemia (IDNA) increased serum ferritin (sFt in the table) 2.5x more than their placebo group; people with iron deficiency and anemia (IDA) improved ferritin levels almost 4x more than their placebos. Neither group got anywhere close to the ferritin levels of the no-deficiencies group. The treatment group was given 160 mg of ferrous iron daily.
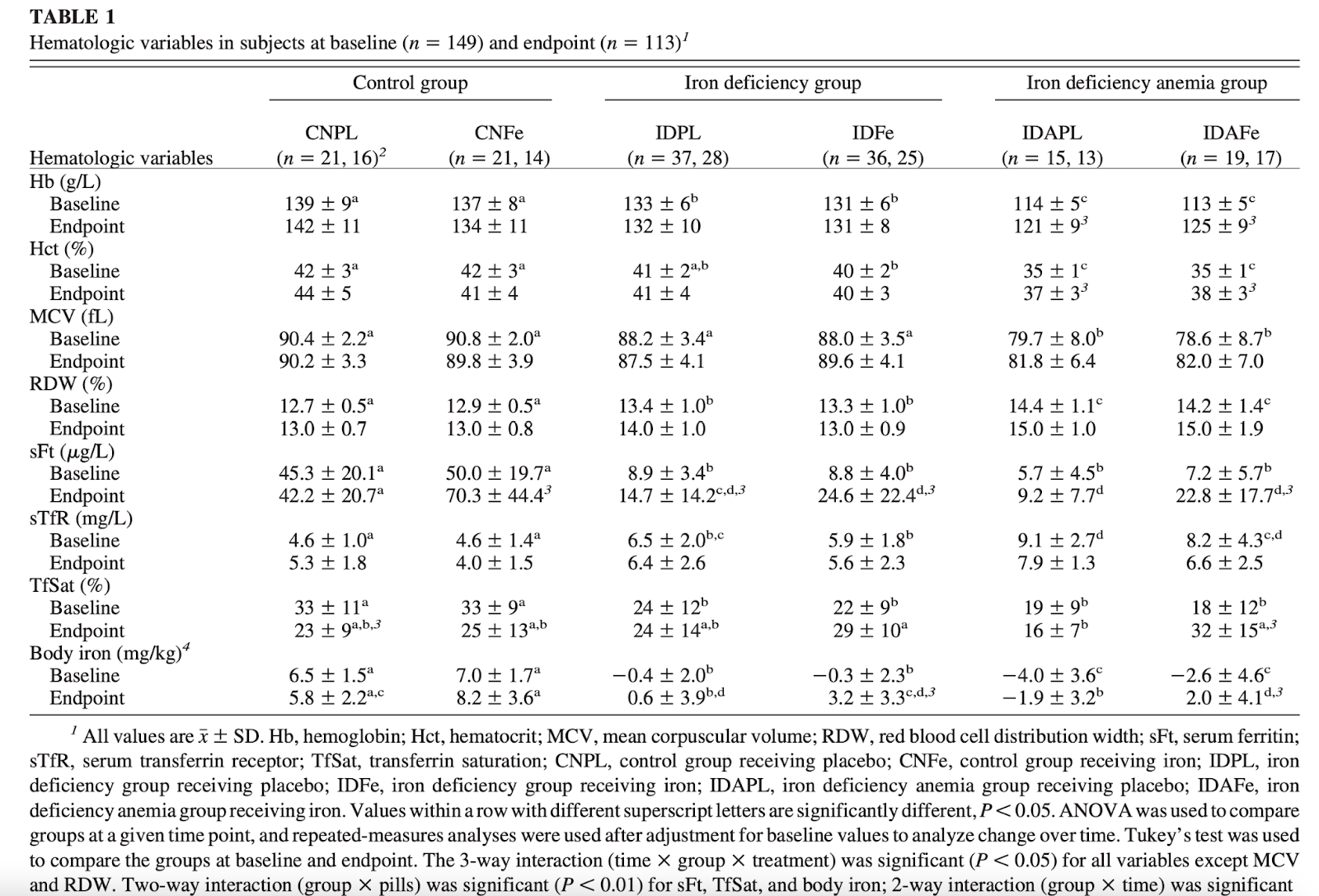
In baseline cognitive testing, IDNA women scored about the same or slightly worse as healthy women, and IDA women scored much worse than both. This is probably an underestimate of the effect, because the study was heavily recruited from students at a single university, who can be expected to be selected for the same range of competence.
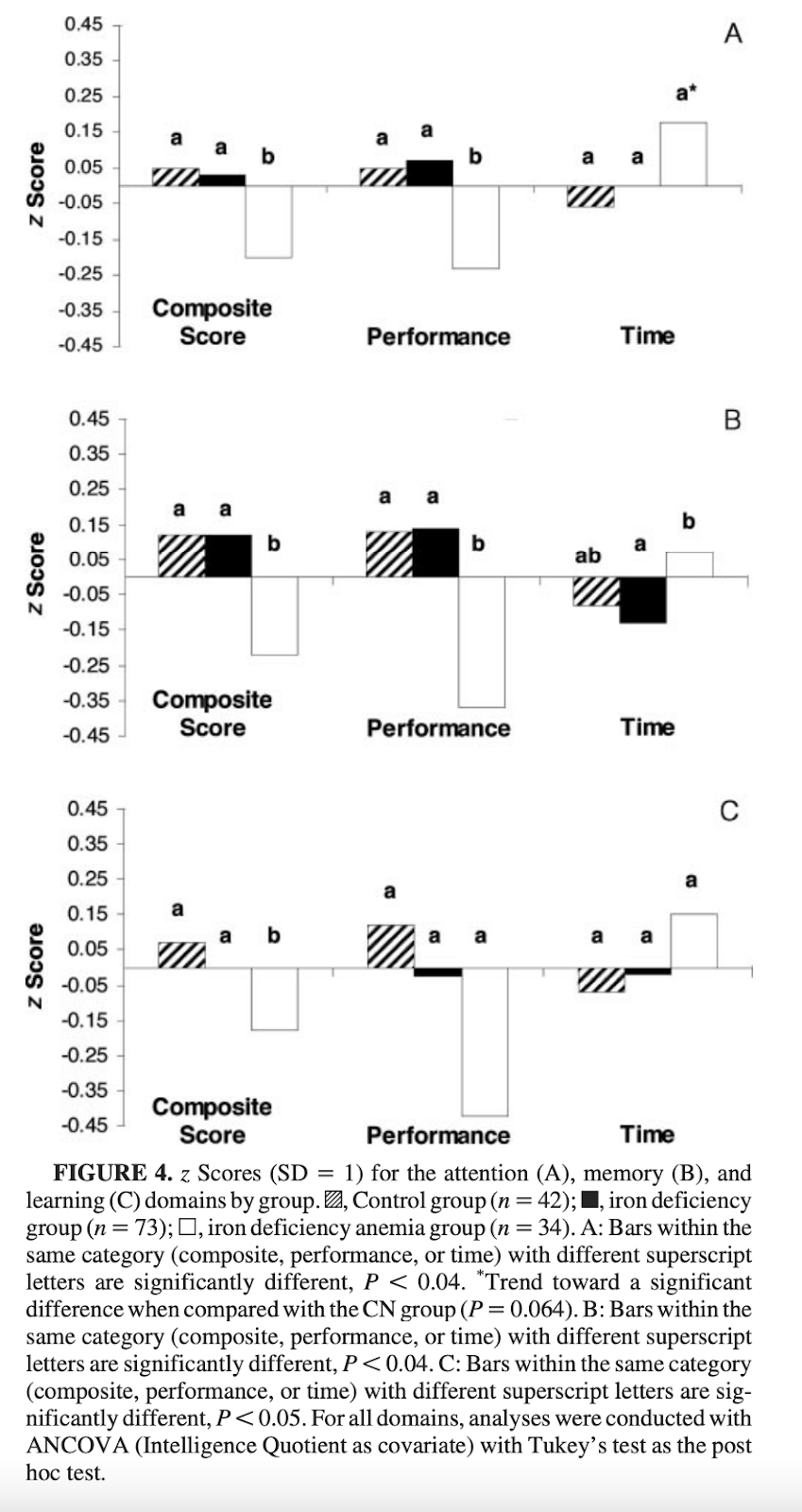
The study separately evaluated treatment-group women who had increased ferritin levels from those who didn’t. The former group had large improvements in their cognitive test results, the latter very modest ones. I think separating out non-responders is fair: if there’s a problem interfering with iron absorption that doesn’t tell you anything about the effect of increasing ferritin levels, and I am studying this mostly for the benefit of people with insufficient dietary intake.
Among ferritin responders, attention, memory, and learning increased from .5 to .75 standard deviations (although somehow that .75 is at p<0.07). That effect size is the equivalent of 7.5-12.5 IQ points or 1.1-1.6 inches in height. Of course the test could be bullshit, but it’s not out of line with anecdotes I hear. Additionally, the treatment groups did not reach the ferritin levels of the healthy group, indicating potentially more gains to be had.
Hemoglobin responders also saw more improvement than non-responders, but the effect size was smaller than with ferritin, indicating an effect of iron beyond increasing hemoglobin.
(Note that the axis has changed from performance to time required, making negatives good. Yes, I am suspicious that they presented total score for one metric and time to completion for another).
Physical
Zhu and Haas (1998)
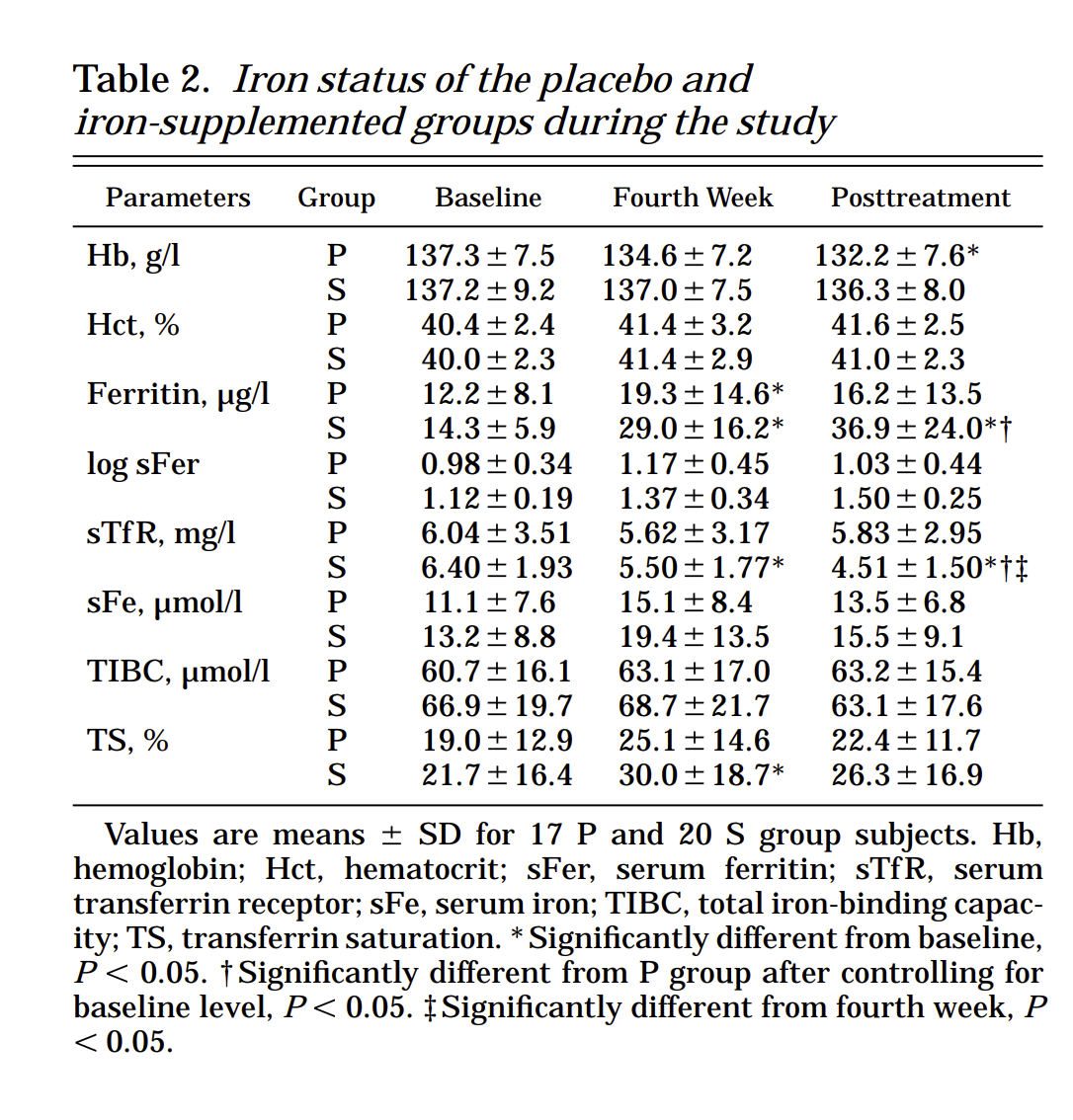
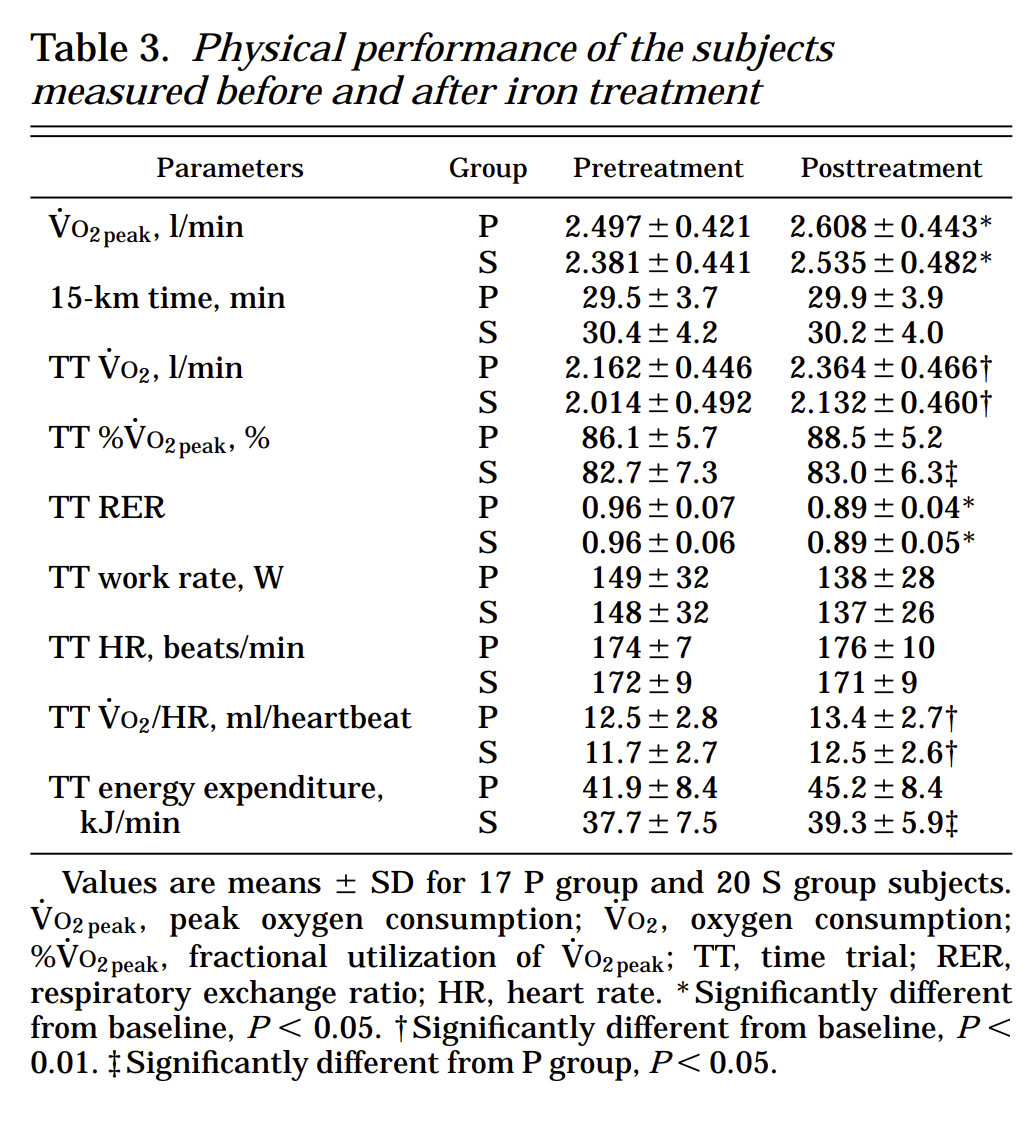
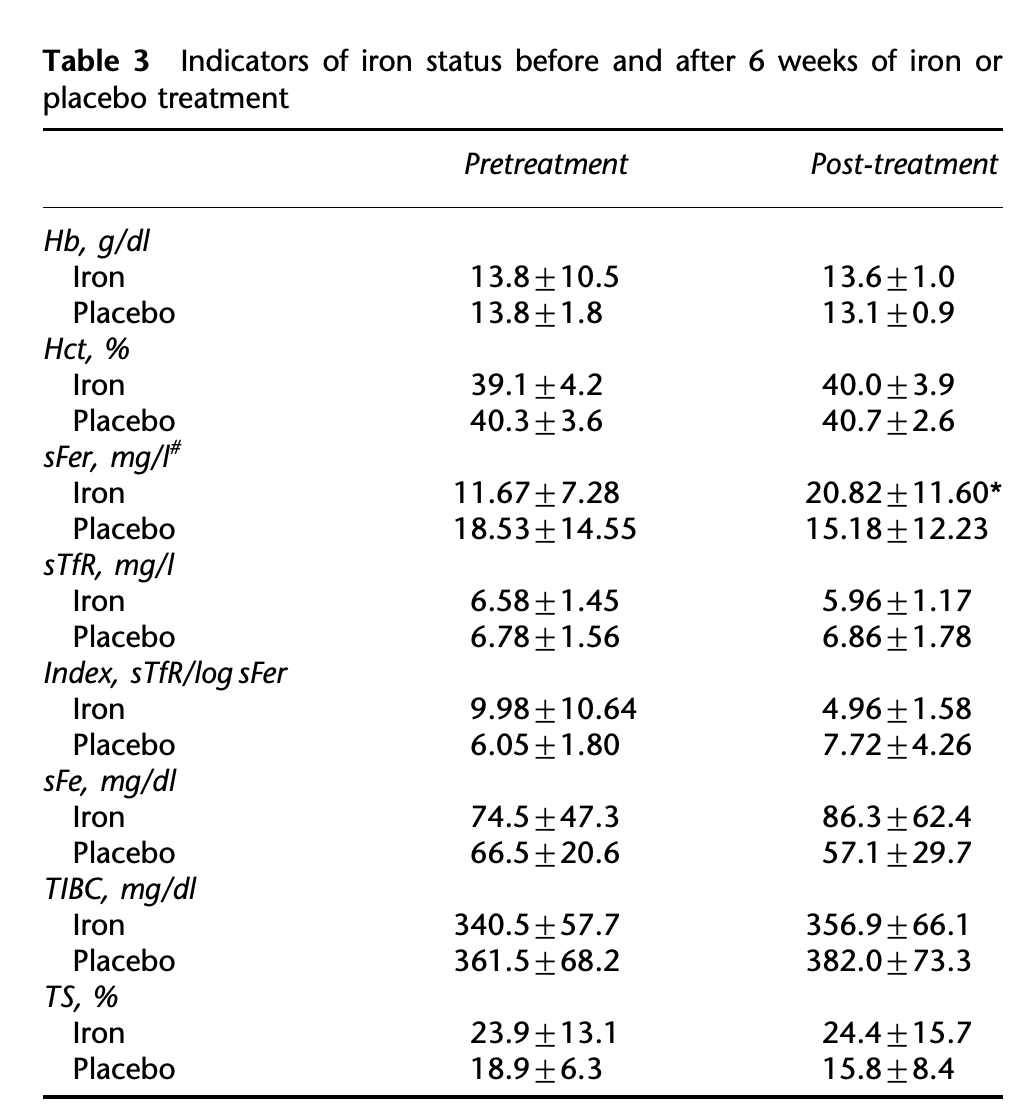
20 women with normal hemoglobin (Hb >120 g/l) but low ferritin (serum ferritin <= 16 ug/l) were given 135 mg ferrous iron supplements for eight weeks and instructed to take with citrus juice. 17 women were given placebos as a control (random assignment, double-blinded). They were given both blood and athletic tests before and after treatment.
Treatment group hemoglobin and iron binding capacity were unchanged. Serum ferritin was up 250% for the treatment group (compared to 30% for the control). Their athletic test results did not improve any faster than the controls, however they needed less energy (2.0kj/min) and oxygen (5%) to get those same results.
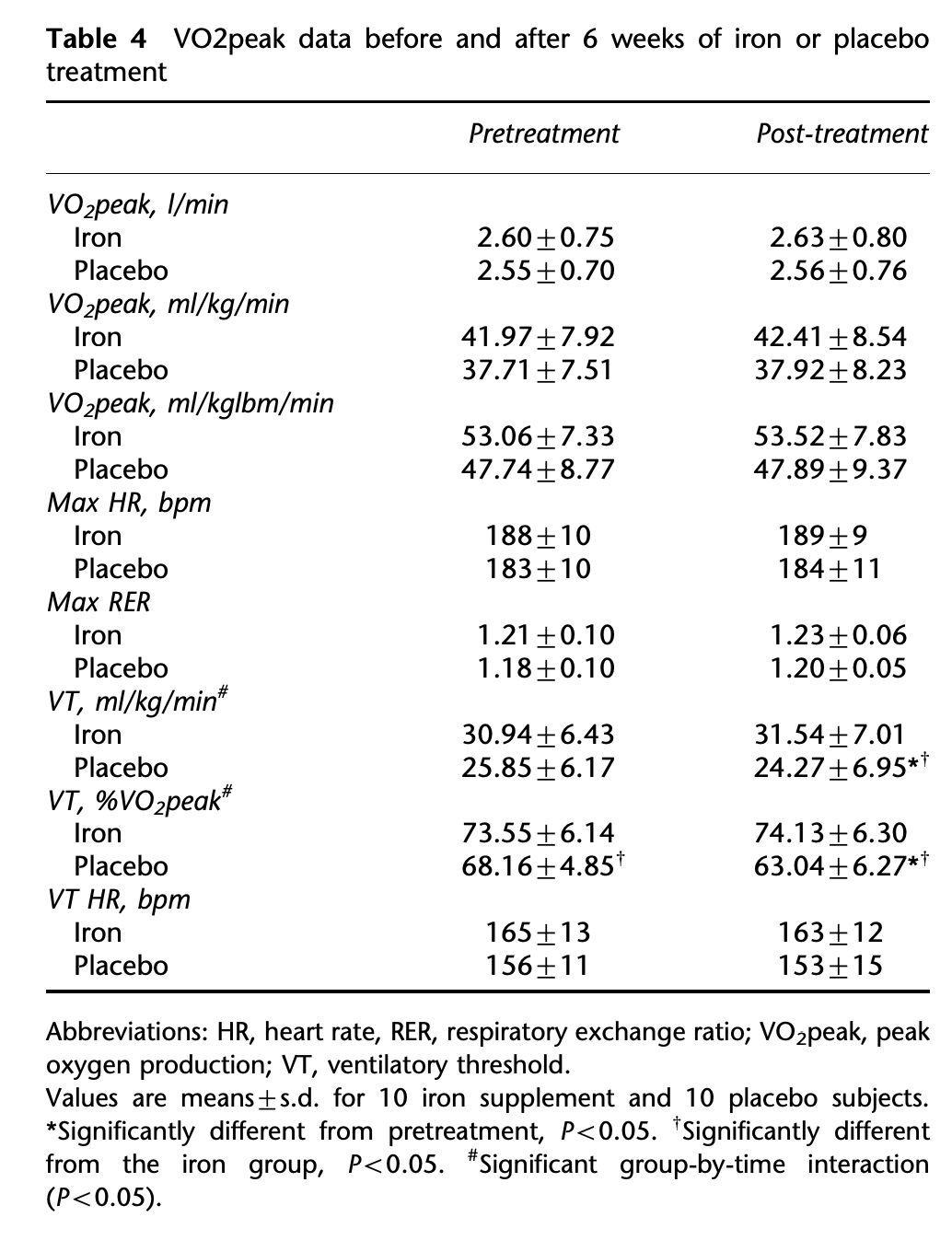
Hinton et al (2000)
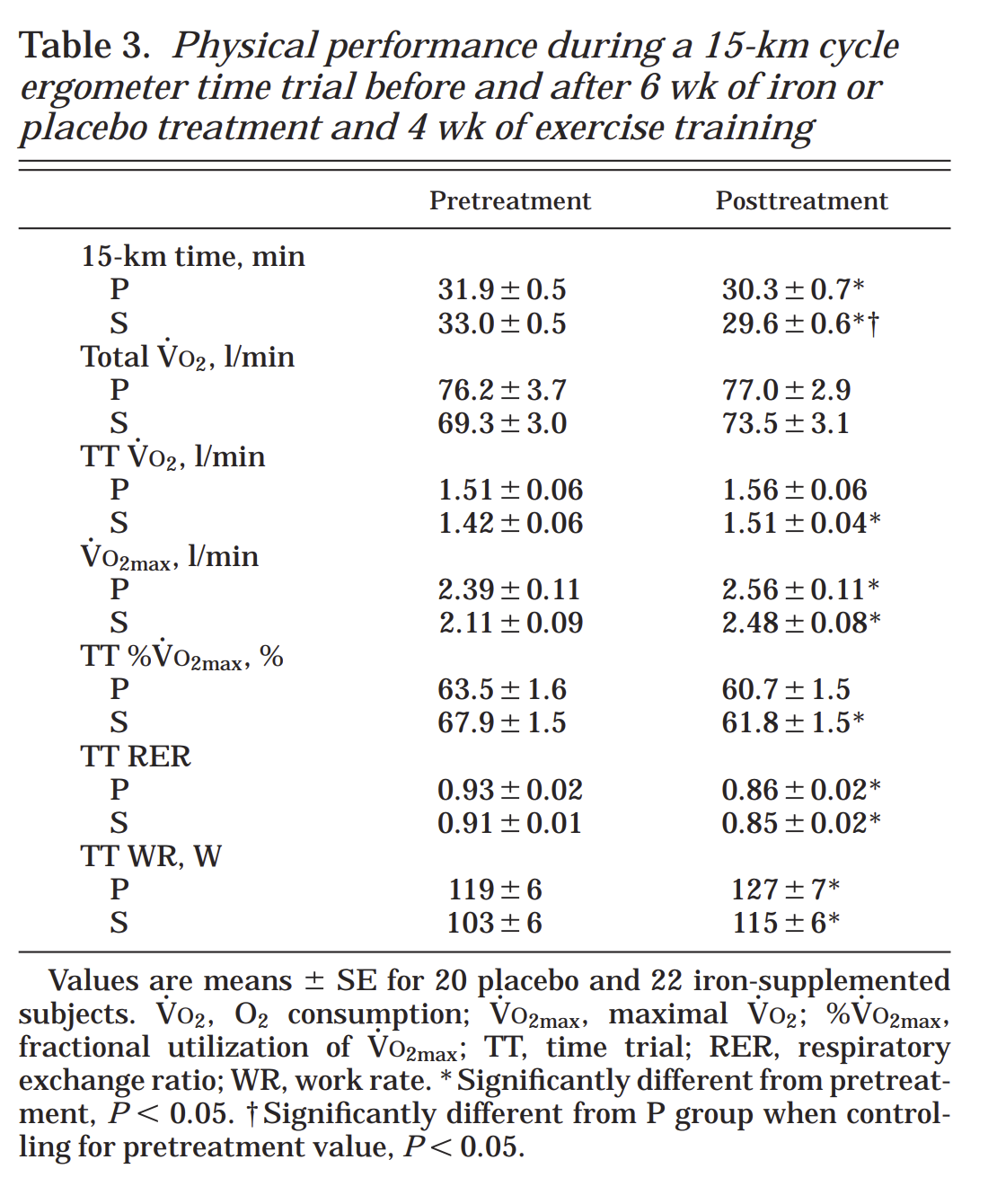
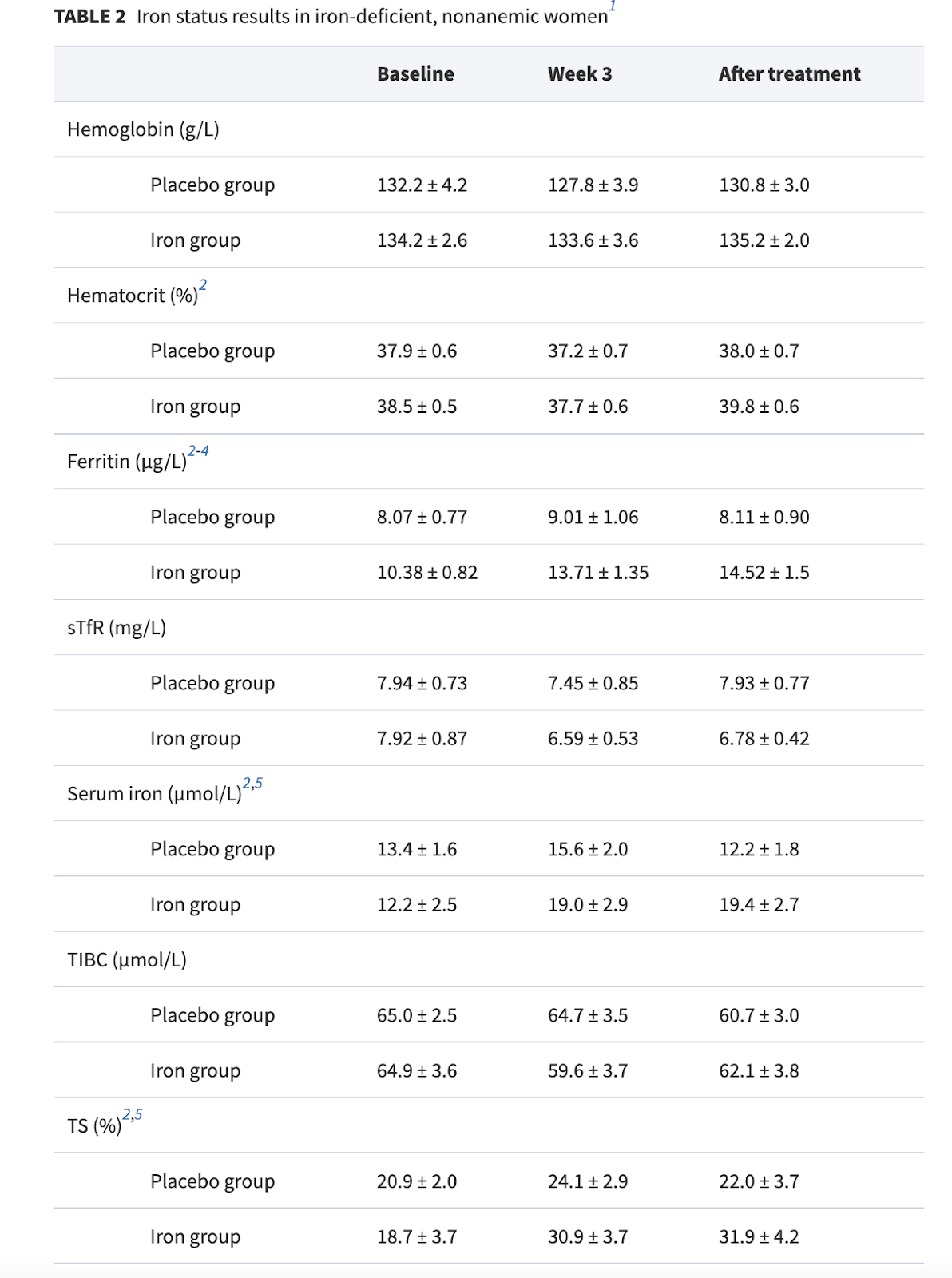
22 women with normal hemoglobin (Hb >12 g/dl) but low ferritin (serum ferritin <= 16 ug/l) were given 100mg ferrous iron supplements for six weeks. 20 women were given placebos as a control (random assignment, double-blinded). They were given both blood and athletic tests before and after treatment.
Iron supplementation did not change hemoglobin or iron binding capacity levels, but did increase serum ferritin by about 50%, and transferrin saturation by 70%. Note that their ending ferritin levels (19.4) were still barely above the bottom of the reference range, indicating there was probably much more room for growth.
The control group went marginally up on some measurements and marginally down on others, I’ve treated their changes as noise.
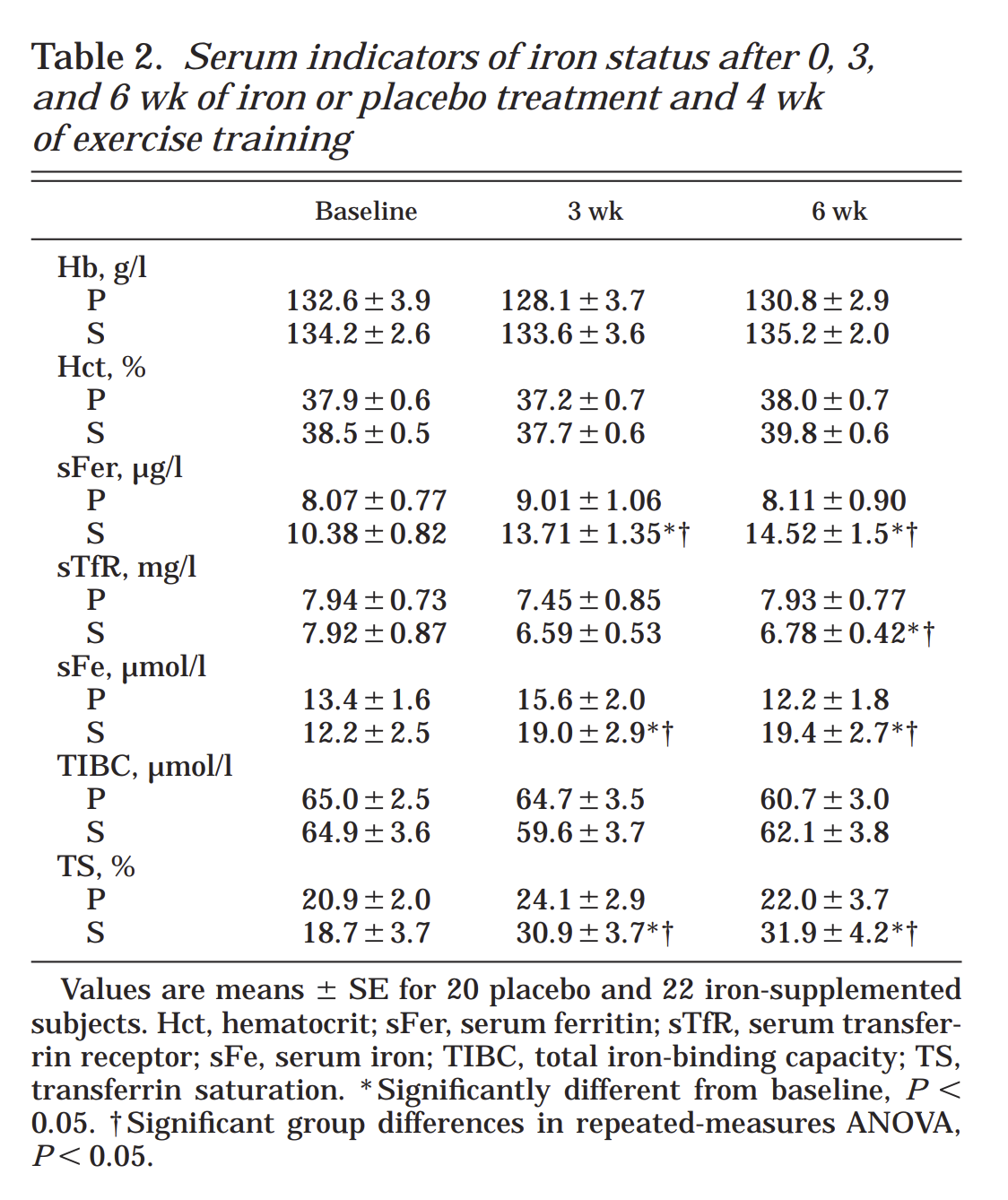
Both treatment and placebo groups were given 4 weeks of exercise treatment; the treatment group showed about double the athletic improvement. Endurance saw a bigger improvement than initial performance.
Brownlie et all (2004)
~20 women, with serum ferritin concentration < 16 ug/L and a hemoglobin concentration > 120 g/L were given 100mg ferrous iron/day for 6 weeks. Of that, 4 weeks also included exercise training.
Once again we see an improvement in ferritin but not hemoglobin or binding capacity.
The treatment group experienced ~30% more improvement in their trial times than the control, or 800% if they started with elevated ferritin. I’m suspicious of this posthoc subgroup analysis, but on the other hand, the bar in this graph is very big.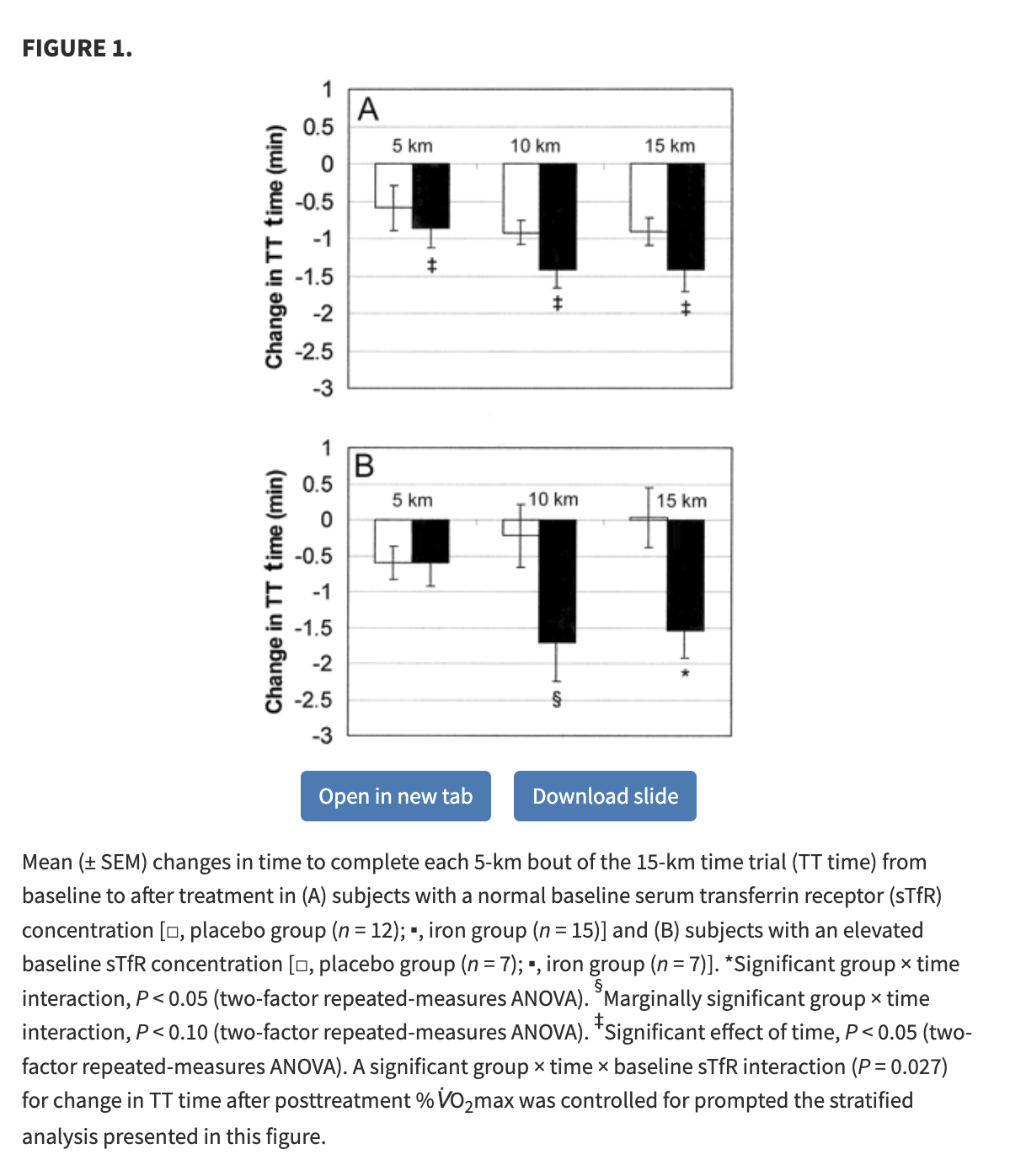
Hinton and Sinclair (2006)
The good news: this study has men! I did not think I was going to find any of those!
The bad news: this study has 20 people, total.
No meaningful change in hemoglobin or binding capacity, near doubling of serum ferritin in the treatment group, 15% drop in ferritin in the control group.
Results are basically identical for the control and placebo groups.
Prevalence Data
Estimates for the prevalence of iron deficiency vary a lot by study and population.
In the first paper I found, the estimate was 9-22% among menstruating women in the general public, and 1-2% among adult men (non-menstruating women were not included but I expect “do you lose 2-4 tablespoons of blood every month?” and “do you occasionally host demanding parasites?” to be more important than hormones or gender identification). Note that this number includes both anemic and non-anemic iron deficiency.
Vegans are at much more risk. One German study of vegan women found a median serum ferritin level of 14 ug/L, a level that is above their reference range and LabCorp’s but below the cut-off in several of the studies cited above. They found 40% of young women fell below their threshold for deficiency (12ng/ml) and 11% of older women (presumably mostly post-menopausal) did so. Women taking iron supplements were excluded from this study.
A second German study (why are they all from Germany?) that allowed supplements and had an even gender split found rates of iron deficiency slightly lower in vegans than omnivores, but both had higher means than anyone in any of the impact studies I found. Nonetheless, 10% of vegans were iron deficient.
My own study (data forthcoming) had 3-4 male vegans and a deficiency rate of 25%-75%, depending on how you count.
Thank you to the Survival and Flourishing Fund for funding this research and Lightcone Infrastructure for providing a home for it.
Thanks to Andrew Rettek for help making my normally very in-the-weeds style more accessible.

Thanks a lot for writing this post!
Personal experience: When I tried a vegan diet, I experienced gradually decreasing energy levels and gradually increasing desire for iron-rich animal products (hamburgers). My energy levels went back to normal when I went ahead and ate the hamburgers.
So, I'm really excited about the potential of nutritional investigations to improve vegan diets!
For bivalvegans, note that some bilvalves are rich in heme iron (heme iron, from animals, is more easily absorbed than the non-heme iron found in plants).
Again, personal experience: I've found that if I'm still feeling tired after multiple days of rest, consuming food with significant heme iron usually solves the problem. (Think this might have been true one time even when I didn't meet the technical criteria for iron deficiency?)
But, just to reinforce the point that too much iron can also be bad:
Source.
Thanks for writing this! I especially appreciated the line "so I looked up studies until I got tired", in context.
Did I understand right that when you said "links are affiliate", this means you earn money if someone clicks on them and buys something? If so, I feel quite strongly that this disclaimer should come before any links, and ideally that affiliate links should be starred.
This is awesome, thank you so much for writing it. Incidentally I wrote a piece on treating restless legs syndrome (RLS), step 1 of which is “fix iron deficiency”: https://henryaj.substack.com/p/how-to-treat-restless-legs-syndrome
I found this a bit hard to read maybe because my biology literacy isn't strong enough. I also skipped the details...
I didn't quite understand why iron deficiencies are "very bad". Here's how I understood it. Is this what op refers to as very bad? 1)
Do you mean bad on a society scale or is it pointed at the reader?